Home » Funded projects »
Beta cells: replace, protect, regenerate
Professor David Hodson, Dr Ildem Akerman and Dr Johannes Broichhagen’s Beta Cell Therapy Programme Grant project
Home » Funded projects »
Professor David Hodson, Dr Ildem Akerman and Dr Johannes Broichhagen’s Beta Cell Therapy Programme Grant project

Led by Professor David Hodson, at University of Oxford, Dr Ildem Akerman, at University of Birmingham, and Dr Johannes Broichhagen, at Leibniz FMP, this project will pioneer new approaches to make better beta cells ready for transplantation, protect the beta cells from an immune attack, and to regrow beta cells inside the pancreas. This research could speed up progress to making life-changing beta cell therapies available for people with type 1 diabetes.
For people living with type 1 diabetes, a cure is likely to mean a combination of different treatments. We need to replace insulin-making beta cells that have been destroyed by the immune system, so people can start to make their own insulin again. And we need to protect new cells from an immune system that is primed to seek out and destroy them.
To reach this goal, scientists are pioneering methods to grow new beta cells in the lab and transplant them into people with type 1 diabetes. Scientists can do this using stem cells. Stem cells have the special ability to become just about any cell in the body, including beta cells. But at the moment, beta cells made from stem cells just aren’t as good at controlling blood sugar levels as real beta cells and don’t survive for long enough. Because of these challenges, scientists are also exploring treatments that could trigger new beta cells to regrow directly inside the pancreas.
Once we can give people with type 1 working beta cells, we also need to protect them from the type 1 immune attack. Treatments, called immunotherapies, are designed to do this by retraining the immune system.
Professor Hodson, Dr Akerman and Dr Broichhagen are hoping to make transformational progress in all three of these areas with the help of two molecules known as incretin receptors. These receptors are found on the surface of beta cells and act as on-off switches to help control the release of insulin. Scientists have already harnessed their potential and developed type 2 diabetes drugs that target the receptors, to help people lower their blood sugar levels. They think the receptors could be key to unlocking major progress in type 1 diabetes beta cell therapies too.
The team has previously discovered that around 20% of lab-made beta cells have incretin receptors on their surface, and that these are better at producing insulin than beta cells without it.
First, the team will develop a way to find the cells that have the receptors, using a technique called cell sorting. If this method was used to analyse a smoothie it would be able to tell us what fruits were used to make it and locate them. Then to check how well they are working, they’ll transplant the receptor beta cells into mice with type 1 diabetes and test if they work better than beta cells without these receptors.
The team will design an immunotherapy that will seek out and bind to incretin receptors at the surface of beta cells, so the treatment goes straight to where it’s needed. They’ll investigate if this precision delivery makes the immunotherapy more effective at slowing or stopping an immune attack, and brings fewer side effects, in mice with type 1 diabetes.
Alpha cells produce a hormone that raises blood sugar and are left unharmed by the type 1 immune attack. They carry incretin receptors on their surface. The research team will modify existing drugs that target incretin receptors to carry cargo that works to change the identity of an alpha cell into a beta cell.
Beta cells therapies have the potential to transform how we treat type 1 and to form part of a cure. Selecting for the top performing lab-made beta cells and arming them with a protective immunotherapy will be key in moving transplants from the lab towards the clinic. While enticing new beta cells to grow inside the body could give us another way of restoring people with type 1’s own insulin production.
Bringing back beta cells would allow us to say goodbye to insulin injections and pumps, reduce the need for constant blood sugar monitoring and help prevent diabetes complications.
Professor David Hodson said:
“During the past decade, a lot of our work has focused on insulin-boosting molecules found on beta cells, called incretin receptors, which have become major drug targets for type 2 diabetes and obesity therapy. Using our knowledge and innovative technologies, we will now translate our work in type 2 diabetes and leverage the potential of incretin receptors in the type 1 diabetes space.
“We’ve developed an ambitious three-prong research programme that spans beta cell replacement, protection and regeneration, so as to give us the best chance of driving discoveries that could make these treatments available for people living with type 1 diabetes.”
Professor Francesca Spagnoli, Dr Rocio Sancho and Professor Molly Steven’s Beta Cell Therapy Programme Grant project

Professor Francesca Spagnoli and Dr Rocio Sancho at King’s College London, together with Professor Molly Stevens at University of Oxford, hope to unlock the full potential of transplants of insulin-making beta cells. They’ll innovate ways to keep cells safe from harm once they’re transplanted into someone with type 1, so we can move closer to the day when beta cell transplants can free people from the relentless task of managing type 1 diabetes.
Scientists are using stem cells to develop treatments to replace the beta cells that have been destroyed in people living with type 1 diabetes. Stem cells have the special ability to shape-shift into other types of cells in the body, including beta cells.
Small clinical trials of stem cell-turned beta cell transplants are now underway and are showing early promise. But after being transplanted into people with type 1 diabetes, new beta cells struggle to survive and gradually lose their ability to make enough insulin and tightly control blood sugar levels.
Using expertise from different fields including biology, immunology and engineering Professor Spagnoli, Dr Sancho and Professor Stevens will lead a team to tackle these challenges and give lab-grown beta cells the tools they need to survive and do their job after transplant.
The team will explore ways to both create tougher beta cells that can better withstand their post-transplant environment, and to make this environment friendlier.
Creating the ideal conditions that keep transplanted beta cells alive and kicking could help us move quicker towards a new era in type 1 diabetes, where people are free from the burden of taking insulin, the fear of hypos and complications, and the mental load of self-managing their blood sugar levels.
Professor Francesca Spagnoli said:
“The Type 1 Diabetes Grand Challenge funding means we can explore new avenues in diabetes research. We’ll be able to start moving some of our discoveries closer to clinical applications and drive improvements in cell replacement therapies, which could ultimately cure type 1 diabetes.”
Professor Shareen Forbes and Dr Lisa Whites’ Beta Cell Therapy Programme Grant project

Professor Shareen Forbes, at University of Edinburgh, and Dr Lisa White, at University of Nottingham are exploring better and more innovative ways to transplant islets, clusters of pancreas cells, into people with type 1 diabetes to enable them to make their own insulin. This could pave the way for wider use of this life-changing treatment, while also making islet transplants much more effective.
In an islet transplant, clusters of cells (called islets) from a donor pancreas are transplanted into someone with type 1 diabetes and start to produce insulin. They’re currently offered to some people with type 1 diabetes who have severe hypos and no awareness of them. However, usually about 60% of the donor cells die soon after transplant.
This means lots of donor islets are needed to have an impact on blood sugar levels. But with a limited number of donor pancreases available for islet transplantation, very few people with type 1 diabetes can currently benefit.
What’s more, islet transplants aren’t as effective as they could be. They rarely allow people to produce enough insulin to stop insulin therapy. And people need to take anti-rejection drugs to prevent their bodies rejecting the donor cells, which can bring serious side-effects.
Scientists are looking at ways to improve the benefits and availability of islet transplants, so they can become part of a cure for type 1 diabetes. Professor Forbes and Dr White think drugs packaged inside microparticles could provide an answer. Microparticles are tiny particles that help to protect a drug from the harsh environment in the body and deliver it to exactly where it’s needed. If drugs that keep islets healthy and protect them from the immune system could be transplanted alongside islets, it could help them to survive and thrive for longer.
Professor Forbes and Dr White will package microparticles with immune-altering and other drugs to improve the survival of transplanted islets. They will test different combinations of drugs in islet transplants in mice, to see which work best to help islets survive and control blood sugar levels.
The team will then run experiments to investigate how to scale up the dose of the drugs and how the treatment might work in humans.
Finally, they will check if the most promising drug microparticle combinations also work to protect beta cells that have been grown in the lab from stem cells.
At the moment only a tiny fraction of people living with type 1 diabetes are eligible for islet transplants. And they’re far from a permanent or perfect fix.
If the team can improve the survival of donor islets it could unleash the benefits of islets transplants – making them much more effective at managing blood sugar levels, eliminating the need for anti-rejection drugs and opening them up for more people with type 1 diabetes.
In the longer-term, their discoveries could also be used to radically improve transplants of lab-made beta cells. This would entirely remove the supply problem of using donor cells, so that in the future everyone with type 1 diabetes could benefit from transplants.
Professor Shareen Forbes said:
“I hope the Grand Challenge’s investment will give people living with type 1 diabetes hope that a cure can be achieved in their lifetime.
“The funding has allowed scientists from diverse fields to come together in this project with a common goal of doing some truly innovative research that will advance the field. By improving the benefits of human pancreas cell transplants, and in time transplants using stem cells, we hope to contribute towards a future where people with type 1 diabetes can live a life free from insulin injections.”
Professor Shanta Persaud and Professor Aileen King’s Beta Cell Therapy Programme Grant project

Professor Shanta Persaud and Professor Aileen King are world-leading experts at studying how insulin-producing beta cells work and develop in humans. They’ll use their specialised knowledge to run state-of-the-art experiments and find ways to improve methods to engineer new beta cells in the lab, so they act and react more like real human beta cells. This project could help to accelerate progress towards life-changing new treatments that restore insulin production in people with type 1 and bring us closer to a cell-based cure for the condition.
People with type 1 diabetes rely on insulin injections or pumps to replace what the immune system has destroyed. While insulin therapy is lifesaving, current insulins don’t come close to the minute-to-minute adjustments that beta cells make to manage blood sugar levels.
Scientists have been trying to find ways to give people with type 1 new beta cells, by making them in the lab from stem cells and transplanting them inside the body. Although lots of progress has been made in recent years, lab-made cells just aren’t as good at producing insulin or responding to changing blood sugar levels as real beta cells are.
Lots of what we know about turning stem cells into beta cells is based on how beta cells develop in mice. But Professor Persaud and Professor King have been studying human pancreas development and want to harness this knowledge to make better performing beta cells that are well equipped to survive transplantation.
Professor Persaud and Professor King will lead a team to:
They’ve discovered that cells that support nerve cells (called Schwann cells) may also help support beta cells. They will carry out tests to see if Schwann cells could improve the ability of stem cells to transform into functioning beta cells.
Once beta cells have been made, the team must make sure they are an elite class of insulin producers. They’ll run tests to see what type of support, nutrients and special molecules can help the newly made cells work even better.
Next, they’ll use state-of-the-art techniques to rigorously test if the lab-made beta cells are really acting like real beta cells. This includes looking at how the lab-made beta cells use oxygen, store insulin and respond to rising blood sugar levels.
The team will coat clusters of lab-grown beta cells with survival boosting molecules, by a process called nanoencapsulation, and test if this helps them survive transplantation better.
Having an unlimited supply of elite beta cells ready for transplantation could mean a future where people with type 1 diabetes never have to think about their blood sugar levels or insulin, because their beta cells are doing it for them. While transplants would also help to reduce the risk of developing diabetes complications.
If successful, this project will turbo charge progress towards clinical trials of transplants using new and improved lab-grown lab cells, and move us closer to a cure.
Professor Aileen King said:
“People with type 1 diabetes have to constantly think about their blood glucose levels and adjust their insulin doses in response. Our aspiration is to produce fully functioning beta cells suitable to implant into people living with type 1 diabetes, which do this on their behalf.
“This would be transformative for people with the condition, as it would restore the body’s minute-to-minute insulin production that is required to carefully control blood glucose levels – reducing the risk of dangerous blood sugar lows and long-term diabetes complications, while also reducing the huge psychological impact of living with diabetes.”
Dr Danijela Tatovic’s Root Causes Programme Grant project

Dr Danijela Tatovic is a clinical research fellow at Cardiff University who designs early phase clinical trials, which are an important step towards taking science from the lab bench into the clinic. In this Grand Challenge research project, Dr Tatovic will test a combination of two therapies, both already licensed to treat other autoimmune conditions, to see if together, they can help protect surviving beta cells and delay progression of type 1.
Type 1 diabetes occurs when a person’s own immune system mistakenly attacks insulin-producing beta cells in the pancreas. This process is known as an autoimmune response and in people at risk of type 1, it begins long before the symptoms of diabetes appear.
New therapies that help to control these autoimmune responses and prevent or slow the attack on beta cells are showing real promise. One medicine, abatacept helps to stop ‘bad’ immune cells from attacking the beta cells. However, the drug also dampens down ‘good’ immune cells that naturally control the autoimmune response. So, it’s important we have the right balance of them.
Dr Danijela Tatovic’s research is exploring how to overcome this problem. So far, she has shown that in mice with type 1 combining abatacept with another medicine, called IL-2, can help to keep the right balance of immune cells, so beta cells are better protected from the ‘bad’ ones.
Now Dr Tatovic’s’s team wants to understand whether a combination of abatacept and IL-2 works in people with type 1 and to find out what dose and timings of the medicines work best.
The researchers will run a small clinical trial where one group of people with type 1 will receive abatacept over two months, boosted with IL-2. Another group will receive abatacept alone.
To understand more about how the immune cells respond to the medication, the researchers will use state-of-the-art methods and equipment to track where the immune cells are in the body, and when and how they are doing their job.
Dr Tatovic’s is also joining forces with other experts, who will sophisticated mathematical models to analyse the data they collect and to predict which doses of each treatment is likely to be most successful in combination.
Knowing which doses of the combination of drugs are most effective at preserving beta cells will allow the researchers to design a larger clinical trial, involving more people. The next trial will help them to find out whether the therapy can protect beta cells from destruction and prevent or slow progress of type 1 diabetes. In future, it could mean that people at risk of type 1 can be treated before their beta cells have been destroyed, to try to delay or prevent the condition from developing. While disrupting the immune attack in people who’ve just been diagnosed with type 1 could help to keep more of their surviving beta cells alive, so they can make some of their own insulin for longer.
Dr Danijela Tatovic said:
“As a clinical diabetologist, I witness the struggle that people with type 1 diabetes go through on a daily basis to achieve optimal control of their blood sugars. This is changing. We are on the cusp of making fundamental difference to the treatment of type 1 diabetes, from burdensome insulin replacement to preserving a person’s own insulin. I am delighted and very grateful to the Type 1 Diabetes Grand Challenge.”
Dr James Pearson’s Root Causes Programme Grant project

Dr James Pearson is a diabetes researcher at Cardiff University. This Grand Challenge project will allow him to test whether a new medicine, that slows the destruction of beta cells in people with type 1 diabetes, is more effective if administered at a particular time of day.
Type 1 diabetes occurs when a person’s insulin-producing beta cells in the pancreas are destroyed mistakenly by the body’s own immune system. The error occurs, at least in part, because immune cells called Tregs that normally help prevent beta destruction, can’t do their job properly in people who develop type 1.
Medicines designed to help boost Tregs and protect beta cells from destruction are being tested in clinical trials with people who’ve recently been diagnosed with type 1. One of the medicines is a low dose of a protein called IL-2 that helps the population of Tregs grow and do their job effectively. However, although the trial results are promising, for some people, the medicine just doesn’t work.
Dr Pearson’s previous research tells us that the number of Tregs in a person’s blood follows a daily pattern, rising and falling during a single day. He’s also found that these cells can only do their job of policing the damaging immune responses at the root of type 1 at certain times of day. In mice, IL-2 protein is responsible for altering these time-of-day changes in Tregs. When the mice are given IL-2 at 7pm, their Tregs do a better job at preventing beta cell destruction than when the same dose is given at 7am.
Dr Pearson wants to find out whether the differences in Treg activity in the morning and evening can explain why some people with type 1 don’t benefit from the IL-2 therapy. He will explore when during the day Tregs get the biggest boost from the IL-2 in mice, and test whether IL-2 is more effective in the morning or evening at preventing or slowing type 1.
Dr Pearson will also study blood samples from people with type 1 to identify how the Treg activity varies between individuals. He will treat samples of people’s Tregs in the lab with IL-2 to see how it boosts the cells’ ability to control the immune cells that destroy beta cells.
By looking closely at Treg cells in both mice and humans, Dr Pearson and his team will discover why Tregs behave differently at different times-of-day and the best time to give a promising new medicine to best boost Tregs, so they can to do their job better and help to fend off the immune attack in people with or at risk of type 1.
Dr Pearson’s research could mean that in future, IL-2 can be given to coincide with when the body’s cells are most responsive to the therapy. It may lead to a new clinical trial to test a time-of-day-specific low dose IL-2 for people with type 1 and those at high risk of developing the condition.
Dr James Pearson said:
“I am thrilled to receive this funding for our research which will expand our research group and move our research forward into clinical practice. This research will identify how immune cells vary over the course of the day but also how well they respond to therapy. This knowledge will enable us to improve the success of therapies for people with, and at risk of, type 1 diabetes by identifying when best to administer therapy.”
James is recruiting people 18-70 living with type 1 diabetes who can attend the University Hospital of Wales, Cardiff. Taking part would involve giving two blood samples, one in the morning between 7-9am and another 10-14 hours later, at the University Hospital of Wales, Cardiff. Eligible participants who successfully donate both samples will be provided with a £300 voucher from Lovetoshop.
To get involved in this study, please contact the research nurses for further information: Shinto Jose (joses8@cardiff.ac.uk) and Alex Howell (howella4@cardiff.ac.uk).
Professor Sarah Richardson’s Senior Research Fellowship project
Professor Sarah Richardson co-leads the Islet Biology Team at the University of Exeter Medical School. She has been researching diabetes since 2007 and is one of the Senior Research Fellows for the Type 1 Diabetes Grand Challenge. Her project will investigate how and why the immune system destroys insulin-producing beta cells in type 1 diabetes, and how the process may differ between people with the condition.
In her previous research, Sarah showed that the biological processes driving the development of type 1 diabetes are not the same in everyone with the condition and there are different subtypes of type 1 diabetes. She found that the number and type of immune cells that children with type 1 have are different to those present in people diagnosed in their teens or older. When people are diagnosed with type 1 at an older age, they have more beta cells than expected. Sarah thinks this is because some of their beta cells are dysfunctional rather than destroyed.
In this project, Sarah will study pancreas samples taken from people at the early stage of type 1 development to look at differences between people in how their immune system attacks and destroys beta cells. This research will allow the subtypes of type 1 to be better defined.
Knowing the form of type 1 an individual has could help tailor how their diabetes is treated and managed. Sarah’s previous research suggests that the effectiveness of immunotherapy drugs for type 1 will be dependent on their specific form of type 1 diabetes. Sarah hopes to learn more about which treatments might work best for different people by examining how immunotherapy drugs work in each form of type 1. With this knowledge, scientists will be able to work on creating an armoury of new treatments that target different lines of the immune system’s attack, so everyone affected by type 1 can be matched to the best treatment for them.
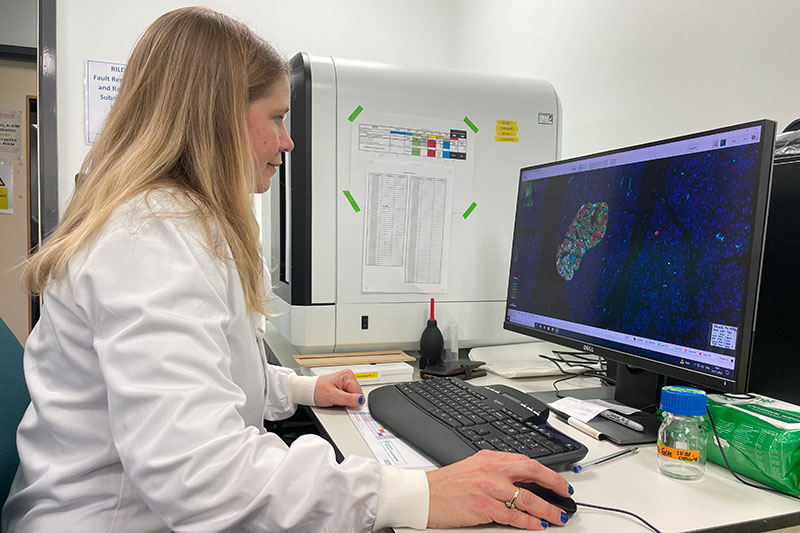
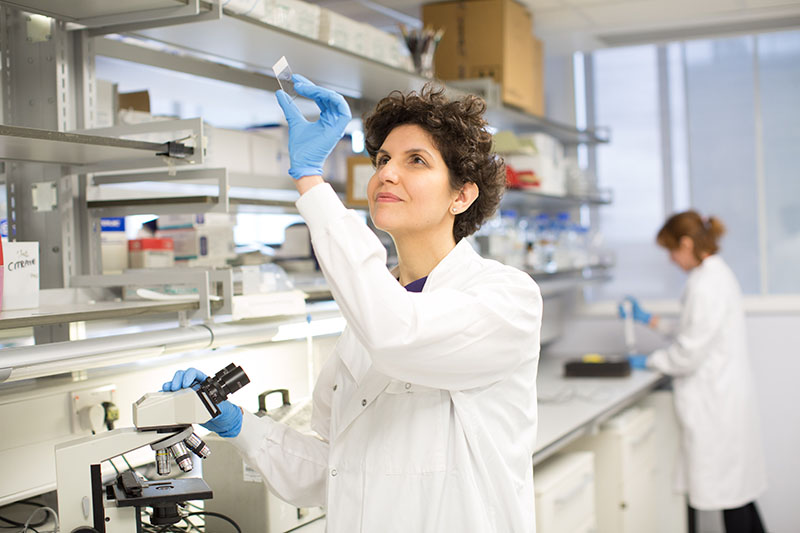
Sarah will also explore how beta cells can fight back against the immune attack and why beta cells in some people with type 1 can survive for many years after their diagnosis. She will use pancreas samples from people with type 1 to explore how beta cells (and the pancreatic islets they are located within) defend themselves against the immune system. To do this, she will use state-of-the-art imaging equipment to look at the samples as well as growing systems of living beta cells and immune cells in the lab. Sarah will investigate a protective layer that surrounds beta cells, called the basement membrane, to understand more about when and how it develops. She’ll also identify molecules made by beta cells that can fortify them against the immune attack.
It is hoped that these insights will be used to develop new treatments to shield beta cells from the immune system attack in type 1 diabetes. If combined with treatments to replace damaged and destroyed beta cells with healthy lab-grown versions or islets from organ donors, this could be a potential cure for type 1 diabetes
Professor Sarah Richardson said:
“As a scientist, one of the things that interests me about diabetes is the way it affects people in extremely different ways. My fellowship will explore how the early development of the pancreas may influence the form of type 1 diabetes a person develops. Ultimately, this will help us tailor existing and emerging therapies to the individual, maximising the benefits for people with type 1 diabetes.
“I also aim to develop a better understanding of how beta cells can protect themselves from the immune attack, which not only holds huge promise for improving beta cell replacement strategies but has the potential to bring us closer to a cure.”
Professor Victoria Salem’s Senior Research Fellowship project
Professor Victoria Salem is the RD Lawrence Professor of Diabetic Medicine at King’s College London. She researches the islets in the pancreas, which is where insulin-producing beta cells and other hormone-producing cells are located. The aim of her Grand Challenge project is to develop a device that can be implanted into people with type 1 diabetes to deliver a new supply of beta cells.
Finding an effective way to replace damaged and destroyed beta cells with healthy, functional beta cells is critical to curing type 1 diabetes. One way of making new beta cells is to grow them in a lab from stem cells, a type of cell which can develop into any other cell type. Trials are ongoing in the US to transplant these lab-grown beta cells into people with type 1. But these patients must take drugs called immunosuppressants (which can have serious side effects) to stop their immune systems attacking these new beta cells.
To overcome the need for immunosuppressants, Vicky plans to hide her lab-grown beta cells inside a soft, jelly-like case. Beta cells need an extensive blood supply to provide them with the oxygen and nutrients they need. So, Vicky needs to create a system that allows nutrients to get to the beta cells, but doesn’t let immune cells in. Once implanted into someone with type 1, this case would keep the precious beta cells safe from the immune system attack which caused their type 1 in the first place. This research could also help protect islets transplanted from organ donors, meaning transplant recipients wouldn’t need to take immunosuppressants.
Vicky and her team will collaborate with researchers at the University of Birmingham to use specialised techniques to create clusters of beta cells from stem cells and find those which are good at releasing insulin.
The next step will be to enclose these beta cell clusters in a supportive water-based medium called a hydrogel. Vicky will work with world leading researchers to develop a hydrogel which can support the beta cells both physically and nutritionally. By experimenting with different materials, they will engineer a sophisticated device which keeps the supporting blood vessels close enough to nourish the beta cells but far enough to prevent immune cell invasion.
Once they are happy with the design, they will print the whole system of protective coating and beta cells in 3D using a high-tech machine called a bioprinter. Vicky said: “Imagine a colour inkjet printer – nozzles eject different coloured ink onto paper, line by line, to build up your document. The nozzles of our bioprinter variously contain our hydrogels and different living cells. We can even print the pattern of hydrogels and cells in precise three-dimensional structures.” She will then test the implant in mice to build the evidence needed to take it into clinical trials with people with type 1 diabetes.
It is hoped this research will lead to the development of a cell-based device which can be implanted into people with type 1 to help them to produce their own insulin again, potentially forming part of a cure for type 1. Within her five-year Fellowship, Vicky hopes her device will be ready to test in early clinical trials of people with type 1.
Professor Victoria Salem said:
“There are so many hurdles to creating a successful cell-transplant for people with type 1 diabetes. We can only crack this by working together – building fruitful collaborations across disciplines and the Grand Challenge is providing the boost we need to mobilise the best scientists in the UK towards this cause!
“I will lead a team of outstanding researchers, and international collaborators, to engineer improved beta cell replacement technologies.
“The dream for a cell-based cure for type 1 diabetes is now tantalisingly close – I’m so excited and honoured to be a part of this journey.”
Professor James Cantley’s Senior Research Fellowship project

Professor James Cantley is a diabetes researcher at the University of Dundee. He is one of the Senior Research Fellows for the Type 1 Diabetes Grand Challenge and specialises in beta cells, the insulin-producing cells in the pancreas. His Grand Challenge research project aims to identify, develop and test new treatments to grow new beta cells, and encourage surviving beta cells to replicate directly in the pancreases of people with type 1 diabetes.
The insulin-producing beta cells in the pancreas are destroyed by the immune system in type 1 diabetes. New treatments are urgently needed to restore beta cell function in people with type 1 so they can make their own insulin again.
James’ research will bring us closer to new treatments to encourage beta cell growth in people with type 1 diabetes. It is hoped these treatments will reverse the lack of insulin in type 1 diabetes. Plus, unlike transplanting lab-grown or donor beta cells, a person’s own regrown beta cells wouldn’t be rejected as foreign cells. This means people receiving this treatment wouldn’t need to take immunosuppressant drugs, which can have dangerous and unwanted side effects. At the end of his fellowship, James hopes to have found drugs that encourage beta cells growth, and which are suitable for testing in clinical trials of people with type 1 diabetes.
Researchers know of some biological processes that drive beta cell growth, but there are gaps in their understanding. In his fellowship, James will try and bridge these gaps. First, he and his team will identify potential drugs (or chemical starting points for drugs) which prompt beta cell growth. The researchers will then switch on and off genes and proteins important for beta cell growth to understand how these drugs work.
Then, they will test the most promising ones in animal and human cells in their lab. Next, they will give the most effective drugs to mice with type 1 diabetes to test whether they can increase insulin production and help to manage blood glucose levels.
As well as studying ways to activate the growth of new beta cells, James will also explore whether it’s possible to clone existing beta cells. In people with type 1, a small number of beta cells sometimes survive the immune attack. A drug being tested for Alzheimer’s disease may be able to help these remaining beta cells multiply. James will give this drug to mice with type 1 to see if it can stimulate their surviving beta cells to multiply and make insulin. James hopes this drug could be used alongside beta cell regeneration drugs to boost beta cell numbers.
Professor James Cantley said:
“Regenerating beta cells in the pancreas has the potential to revolutionise the treatment of type 1 diabetes, by replacing cells destroyed by the immune attack, and ultimately leading to stable blood sugar levels and a life free from insulin injections. However, there are many obstacles to developing successful therapeutic strategies.
“To overcome these, I have put together an ambitious, future-focused project and an outstanding international team of scientists which, with the support and funding from the Type 1 Diabetes Grand Challenge, will enable us to focus on our mission of identifying new strategies to drive beta cell regeneration in the pancreas. We are on the cusp of a new era of type 1 diabetes treatment, and I can’t wait to see where this research takes us.”