The Type 1 Diabetes Grand Challenge is funding £50 million of research to propel us towards a cure and to change the lives of people living with type 1 diabetes. But the partnership has also been life-changing for the researchers who’ve been awarded Grand Challenge funding.
Earlier this year, Professor Sarah Richardson became one of the first exceptional scientists to receive Type 1 Diabetes Grand Challenge funding.
She’s already made tremendous progress, recruiting staff, setting up her lab, forming collaborations and finalising publications. And she still made time to tell us just what our funding means to her and how the Grand Challenge is building a culture that allows UK type 1 diabetes research to thrive.
“This funding has undoubtedly transformed my research and enthusiasm for life and helped me to build a solid team to push forward our important research.”
“The funds have already made a difference to me, to my team, to UK researchers and most importantly, I know this will ultimately make a difference for people living with type 1 diabetes. Thank you for making this possible.”
Before the fellowship, the demands of her job, gave her little time to focus just on research – but thanks to the Grand Challenge, this has changed beyond recognition.
“There were not enough hours in the day, days in the week and weeks in the year. The pressures were such that I was seriously considering what other options were out there for me. Something I was saddened by as my spark comes alive when I have the opportunity to work in this most important of areas, alongside colleagues who are equally driven and motivated by our common want to change lives for the better.”
“Every day is exciting. We are learning new things, developing new skills – I have learnt how to code – to improve our capacity to deal with large, complex datasets.”
Her team immediately swung into action.
“The team have leapt into the project with curiosity and drive, working carefully and conscientiously to advance our knowledge. I am so proud of how their knowledge and skills are developing, and this supportive environment encourages each of them to push their limits.”
But Sarah and her amazing team haven’t stopped there. Thanks to the Type 1 Diabetes Grand Challenge, they’ve been forging new collaborations with other world-leading teams to help translate what they’ve learned in the lab to people with type 1 diabetes.
“The Grand Challenge calls have got people talking, communicating and networking on a whole other level. The excitement and hope this has generated is palpable, and I am so excited to see the outcomes of this over the coming years.”
You may also be interested in
“Thank you” from a Grand Challenge researcher
September 5, 2023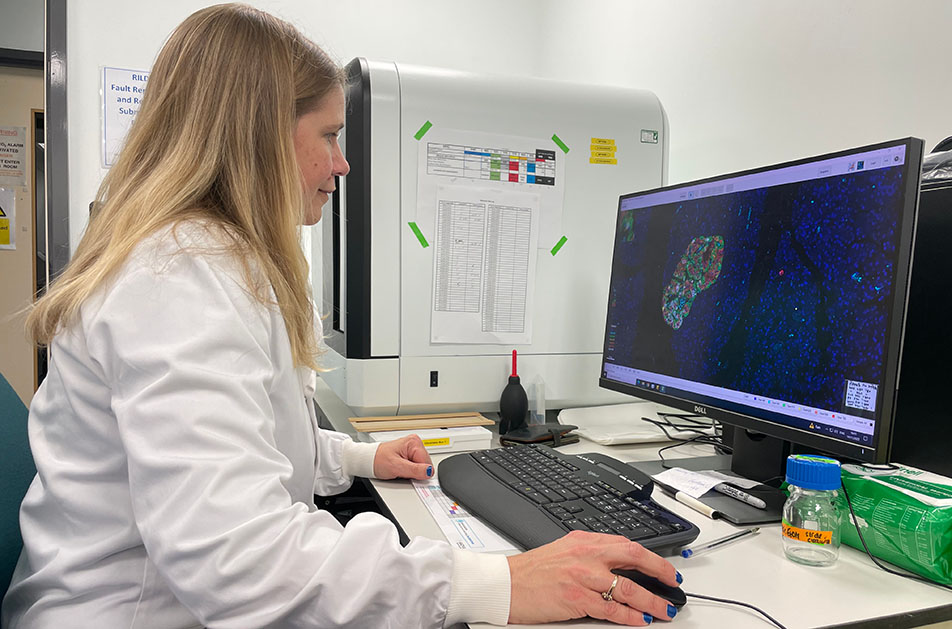
The Type 1 Diabetes Grand Challenge is funding £50 million of research to propel us towards a cure and to change the lives of people living with type 1 diabetes. But the partnership has also been life-changing for the researchers who’ve been awarded Grand Challenge funding.
Earlier this year, Professor Sarah Richardson became one of the first exceptional scientists to receive Type 1 Diabetes Grand Challenge funding.
She’s already made tremendous progress, recruiting staff, setting up her lab, forming collaborations and finalising publications. And she still made time to tell us just what our funding means to her and how the Grand Challenge is building a culture that allows UK type 1 diabetes research to thrive.
“This funding has undoubtedly transformed my research and enthusiasm for life and helped me to build a solid team to push forward our important research.”
“The funds have already made a difference to me, to my team, to UK researchers and most importantly, I know this will ultimately make a difference for people living with type 1 diabetes. Thank you for making this possible.”
Before the fellowship, the demands of her job, gave her little time to focus just on research – but thanks to the Grand Challenge, this has changed beyond recognition.
“There were not enough hours in the day, days in the week and weeks in the year. The pressures were such that I was seriously considering what other options were out there for me. Something I was saddened by as my spark comes alive when I have the opportunity to work in this most important of areas, alongside colleagues who are equally driven and motivated by our common want to change lives for the better.”
“Every day is exciting. We are learning new things, developing new skills – I have learnt how to code – to improve our capacity to deal with large, complex datasets.”
Her team immediately swung into action.
“The team have leapt into the project with curiosity and drive, working carefully and conscientiously to advance our knowledge. I am so proud of how their knowledge and skills are developing, and this supportive environment encourages each of them to push their limits.”
But Sarah and her amazing team haven’t stopped there. Thanks to the Type 1 Diabetes Grand Challenge, they’ve been forging new collaborations with other world-leading teams to help translate what they’ve learned in the lab to people with type 1 diabetes.
“The Grand Challenge calls have got people talking, communicating and networking on a whole other level. The excitement and hope this has generated is palpable, and I am so excited to see the outcomes of this over the coming years.”
“Thank you” from a Grand Challenge researcher
August 10, 2023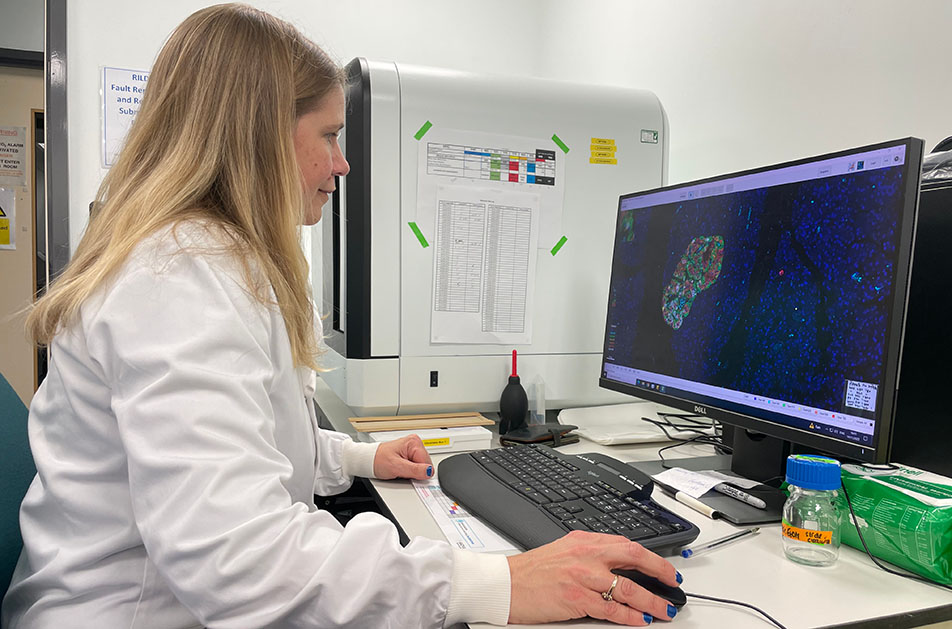
In this podcast produced by DRWF, listen to our Senior Research Fellows, Professor Sarah Richardson, Dr James Cantley and Dr Victoria Salem, as they discuss their research interests, Grand Challenge projects, and the impact funding can have on research.
The Living with Diabetes podcast, produced by the Diabetes Research and Wellness Foundation (DRWF) and hosted by Claire Levy, showcases inspirational stories about diabetes. In episode 22 of the series, the Type 1 Diabetes Grand Challenge takes centre stage, as Claire interviews our three Senior Research Fellows. Hear from Professor Sarah Richardson, Dr James Cantley and Dr Victoria Salem as they explore their specific areas of research and explain how Grand Challenge funding is supporting them to devote more time and energy to their research.
Listen to the recording of the Grand Challenge podcast episode.

Living With Diabetes Podcast 22 – Grand Challenge
Find out more about the funded projects
“Thank you” from a Grand Challenge researcher
August 2, 2023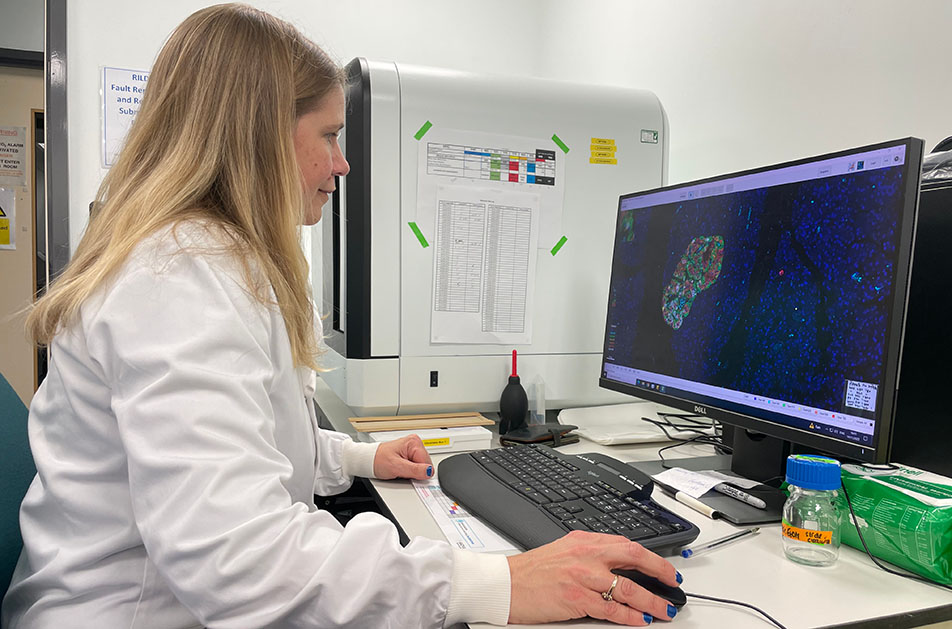
Earlier this year, we kicked off the Type 1 Diabetes Grand Challenge’s £50 million programme of research when we announced the very first scientists who will each solve different problems that could unlock a new era in treatments for people living with type 1. And now, three months later, they’ve already made tremendous progress by recruiting staff, setting up their labs, forming collaborations and even finalising publications. We caught up with them to hear about their research journeys and their hopes for the Grand Challenge.
The Type 1 Diabetes Grand Challenge is funding £50 million of research to propel us towards a cure and to change the lives of people living with type 1 diabetes. But the partnership has also been life-changing for the researchers who’ve been awarded Grand Challenge funding.
Earlier this year, Professor Sarah Richardson became one of the first exceptional scientists to receive Type 1 Diabetes Grand Challenge funding.
She’s already made tremendous progress, recruiting staff, setting up her lab, forming collaborations and finalising publications. And she still made time to tell us just what our funding means to her and how the Grand Challenge is building a culture that allows UK type 1 diabetes research to thrive.
“This funding has undoubtedly transformed my research and enthusiasm for life and helped me to build a solid team to push forward our important research.”
“The funds have already made a difference to me, to my team, to UK researchers and most importantly, I know this will ultimately make a difference for people living with type 1 diabetes. Thank you for making this possible.”
Before the fellowship, the demands of her job, gave her little time to focus just on research – but thanks to the Grand Challenge, this has changed beyond recognition.
“There were not enough hours in the day, days in the week and weeks in the year. The pressures were such that I was seriously considering what other options were out there for me. Something I was saddened by as my spark comes alive when I have the opportunity to work in this most important of areas, alongside colleagues who are equally driven and motivated by our common want to change lives for the better.”
“Every day is exciting. We are learning new things, developing new skills – I have learnt how to code – to improve our capacity to deal with large, complex datasets.”
Her team immediately swung into action.
“The team have leapt into the project with curiosity and drive, working carefully and conscientiously to advance our knowledge. I am so proud of how their knowledge and skills are developing, and this supportive environment encourages each of them to push their limits.”
But Sarah and her amazing team haven’t stopped there. Thanks to the Type 1 Diabetes Grand Challenge, they’ve been forging new collaborations with other world-leading teams to help translate what they’ve learned in the lab to people with type 1 diabetes.
“The Grand Challenge calls have got people talking, communicating and networking on a whole other level. The excitement and hope this has generated is palpable, and I am so excited to see the outcomes of this over the coming years.”
How did you involve people with diabetes when shaping your Grand Challenge research ideas?
Vicky Salem
“For this application, I worked with Alex Silverstein who has type 1 himself, but who has also been the most phenomenal patient advocate over the years through his work with Health Data Research UK.”
James Cantley
“I’ve been a member of a Diabetes UK Diabetes Research Steering Group for 6 years and have also been involved in many public engagement events. Beta cell regeneration regularly features in these discussions.”
“In many ways, I think beta cell regeneration could be the ultimate treatment for type 1 diabetes. We do have a way to go before we see it move from the bench to bedside, but we are on the cusp of a new era of type 1 diabetes treatment, and I can’t wait to see where this research takes us.”
“I’m extremely grateful to those with diabetes who give up their time to help advise and review our research; this input is invaluable to advancing science.”
Sarah Richardson
“Through my work and being a member of a Diabetes UK Diabetes Research Steering Group, I’ve met and become friends with many people with type 1 diabetes, who remain a huge source of inspiration for me.”
“I see the burden; I see the worry. My goal is to make this burden lighter and one day to hopefully remove it entirely.”
“Conversations with people with lived experience of type 1 are always enlightening, humbling and fuel my determination and passion to make a difference.”
How has your Senior Research Fellowship been progressing so far?
Vicky Salem
“We’ve only just started work on the project, but so far, we’ve recruited the most fantastic group of PhD students and postdocs who come from a range of different scientific backgrounds – biologists, biochemists, material scientists and chemists. Together we’ve already managed to grow blood vessels from cells that have been taken from a patient with type 1 diabetes, giving us a single blood sample.”
“We can extract some cells from that blood sample and grow them in the lab and then use those to build brand new blood vessel networks outside the body. This is the start of the skeleton or the backbone we need to introduce the islets to, to then re-transplant them back into that patient.”
“It’s hugely exciting. We can actually see blood flowing through the blood vessels we’re growing in the lab. This kind of an advance applies not only to people with diabetes, but to all sorts of other regenerative medicine approaches.”
James Cantley
“The fellowship has been really helpful in protecting my time and has given me the ability to focus on research fully.”
“The kudos and publicity surrounding the announcement of the Grand Challenge funding has helped me succeed in recruiting three great people to my team, including a research technician, postdoc and PhD student. Advertising the roles as part of the Grand Challenges attracted high quality international candidates with essential skillsets.”
“I’m very excited to begin the next steps.”
Sarah Richardson
“It’s been very exciting to get started! We’ve recruited some amazing people to our team, the new postdoc and research technician have both really hit the ground running.”
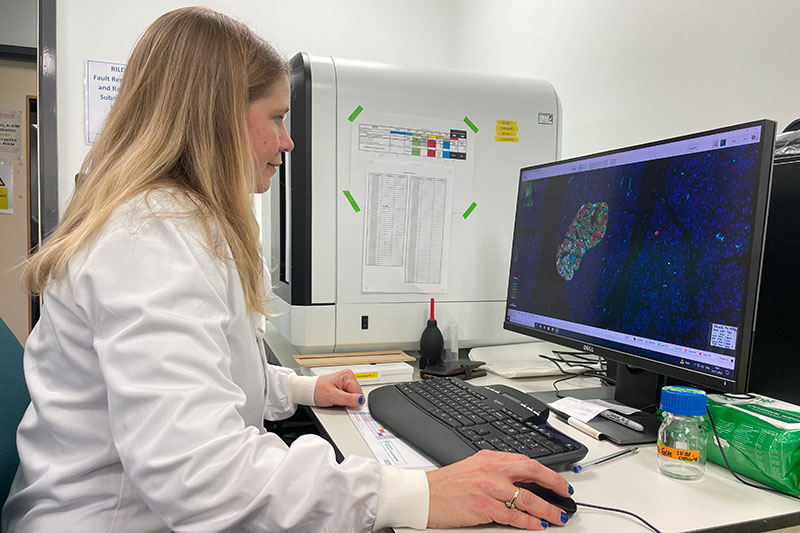
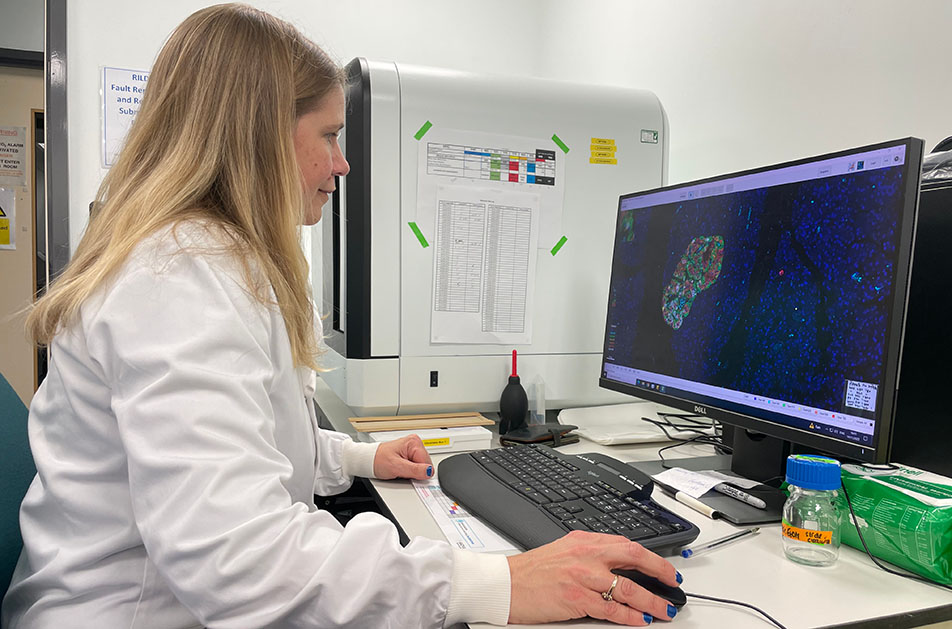
“Together we’ve made a lot of progress, preparing for large-scale imaging analysis and making sure everything is in place for future work. This included upgrading our setup so that up to 10 people can use the software at the same time, both in the lab or remotely. Previously only two people could use it at once and they had to be physically in the lab. This really is a huge step forward!”
“We’ve also collated pancreas images from biobanks around the world, including some very rare samples, allowing us to systematically analyse pancreatic islets in people diagnosed at different ages and stages of type 1 diabetes.”
“We’re also working on getting a few papers submitted to academic journals. The work is fast paced but I’m so grateful to be in this position.”
What is the best thing about your work?
Vicky Salem
“I have the best job in the world. That’s because about 40% of my time is spent with patients, helping them to manage their condition, which is just so rewarding.”
“And of course, talking to patients is incredibly important. There is no point sitting in an ivory tower and coming up with solutions to problems that don’t exist or aren’t important to patients.”
James Cantley
“I’m driven by the excitement of discovering new insights into how the body works, especially the pancreatic beta cell, which has occupied most of my waking hours for the past 20 years.”
“I enjoy the camaraderie and collaborative nature of research, working together towards a common goal, and training the scientists and research leaders of the future. And this Senior Research Fellowship combines all of these!”
Sarah Richardson
“There are less than 700 pancreases available to the research community from people with type 1 diabetes, and even fewer from individuals very close to type 1 diabetes diagnosis where the disease process is most active. Each one looks very different depending on the age someone was diagnosed.”
“One of the best things about my job is spending my day looking at these incredibly beautiful images and working with talented and dedicated researchers to tease out what they can tell us about the root causes of type 1 diabetes.”
Can you tell us about a defining moment in your work as a scientist?
Vicky Salem
“In 2016, I was awarded almost £900,000 of funding from Diabetes UK, to investigate how gut hormones could treat type 2 diabetes and obesity in the future. This was totally life-changing for me because it gave me the opportunity to finish my junior doctor training and become a consultant and at the same time open my own lab and become an independent clinician scientist.”
“At the beginning of this project, I proposed the idea of developing a new way to take images of cells in the pancreas. I remember walking into the room with this huge spinning microscope that cost about £1 million, and thinking, oh my God, where is the on switch?!”
“But even to this day, I remember the first time I saw an image on that microscope of pancreas cells inside a living animal releasing insulin at single cell beta cell resolution, and I thought, yes, I can do this, and I will do this.”
James Cantley
“There have been so many memorable moments in my career, too many to mention! If forced to pick, I would say working on my Diabetes UK-funded PhD project when I was investigating the interaction between oxygen and glucose sensing pathways in beta cells.”
“This was a large project with multiple collaborators, and being involved with so many talented colleagues really underscored the importance of cooperation in science.”
Sarah Richardson
“I will never forget the day I first sat in the lab looking down the microscope reviewing precious donor pancreas tissues, tears streamed down my face as I recognised the loss of so many people, especially children, so far before their time. I want to ensure that we learn from these to improve the lives of those living with type 1 diabetes now and in the future.”
What do you like to do when you’re not working?
Vicky Salem
“I have three children, Georgia is 10, Saul is 11 and Anna is 13, so every bit of spare time I get is focused on them.”
“I have struggled with mum guilt my entire career; I haven’t always been the type of mum that has been at the school gate every day. But I’ve tried to make up for that by talking to them all the time about my work, about the world and encouraging in them the same kind of curiosity that makes my job so fulfilling.”
James Cantley
“When I’m not working, I enjoy spending time with my wife and two daughters, exploring the Scottish Highlands. I’m also a keen climber which helps me to relax and refocus.”
Sarah Richardson
“I have a husband and two daughters, so when I’m not in the lab I take every opportunity to spend time with them and listen to them play music at different open mic nights.”
“I also walk (and run when I can) with my dog, an Australian Kelpie called Mick. Some of my best ideas and solutions to challenges come out of these walks.”
First class research can’t happen without first class researchers, and we couldn’t be more excited to see how the three Senior Research Fellows will break new ground over the next five years.
Find out more about the funded projects
“Thank you” from a Grand Challenge researcher
June 22, 2023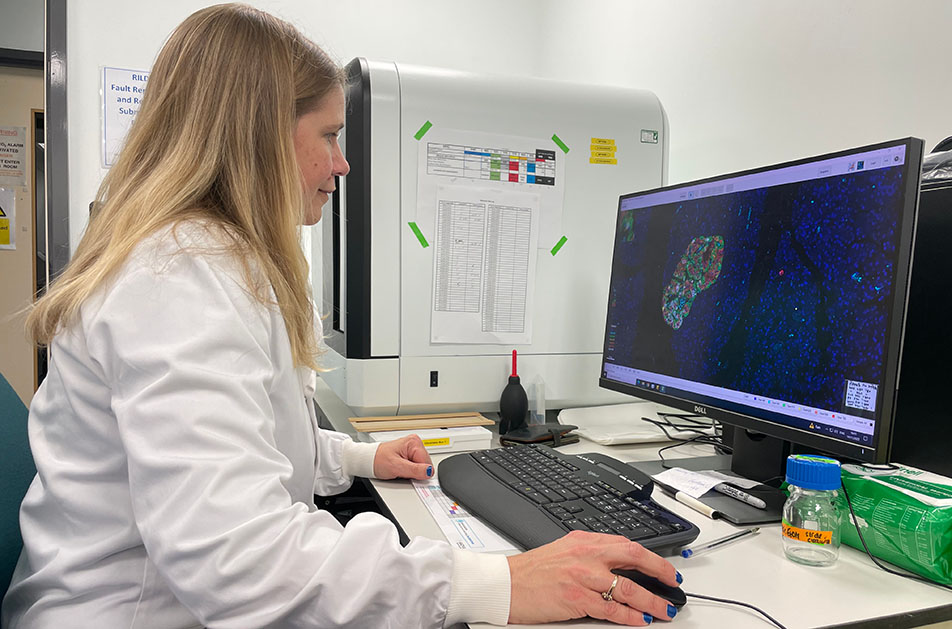
Earlier this year, we kicked off the Type 1 Diabetes Grand Challenge’s £50 million programme of research when we announced the very first scientists who will each solve different problems that could unlock a new era in treatments for people living with type 1. And now, three months later, they’ve already made tremendous progress by recruiting staff, setting up their labs, forming collaborations and even finalising publications. We caught up with them to hear about their research journeys and their hopes for the Grand Challenge.
The Type 1 Diabetes Grand Challenge is funding £50 million of research to propel us towards a cure and to change the lives of people living with type 1 diabetes. But the partnership has also been life-changing for the researchers who’ve been awarded Grand Challenge funding.
Earlier this year, Professor Sarah Richardson became one of the first exceptional scientists to receive Type 1 Diabetes Grand Challenge funding.
She’s already made tremendous progress, recruiting staff, setting up her lab, forming collaborations and finalising publications. And she still made time to tell us just what our funding means to her and how the Grand Challenge is building a culture that allows UK type 1 diabetes research to thrive.
“This funding has undoubtedly transformed my research and enthusiasm for life and helped me to build a solid team to push forward our important research.”
“The funds have already made a difference to me, to my team, to UK researchers and most importantly, I know this will ultimately make a difference for people living with type 1 diabetes. Thank you for making this possible.”
Before the fellowship, the demands of her job, gave her little time to focus just on research – but thanks to the Grand Challenge, this has changed beyond recognition.
“There were not enough hours in the day, days in the week and weeks in the year. The pressures were such that I was seriously considering what other options were out there for me. Something I was saddened by as my spark comes alive when I have the opportunity to work in this most important of areas, alongside colleagues who are equally driven and motivated by our common want to change lives for the better.”
“Every day is exciting. We are learning new things, developing new skills – I have learnt how to code – to improve our capacity to deal with large, complex datasets.”
Her team immediately swung into action.
“The team have leapt into the project with curiosity and drive, working carefully and conscientiously to advance our knowledge. I am so proud of how their knowledge and skills are developing, and this supportive environment encourages each of them to push their limits.”
But Sarah and her amazing team haven’t stopped there. Thanks to the Type 1 Diabetes Grand Challenge, they’ve been forging new collaborations with other world-leading teams to help translate what they’ve learned in the lab to people with type 1 diabetes.
“The Grand Challenge calls have got people talking, communicating and networking on a whole other level. The excitement and hope this has generated is palpable, and I am so excited to see the outcomes of this over the coming years.”
How did you involve people with diabetes when shaping your Grand Challenge research ideas?
Vicky Salem
“For this application, I worked with Alex Silverstein who has type 1 himself, but who has also been the most phenomenal patient advocate over the years through his work with Health Data Research UK.”
James Cantley
“I’ve been a member of a Diabetes UK Diabetes Research Steering Group for 6 years and have also been involved in many public engagement events. Beta cell regeneration regularly features in these discussions.”
“In many ways, I think beta cell regeneration could be the ultimate treatment for type 1 diabetes. We do have a way to go before we see it move from the bench to bedside, but we are on the cusp of a new era of type 1 diabetes treatment, and I can’t wait to see where this research takes us.”
“I’m extremely grateful to those with diabetes who give up their time to help advise and review our research; this input is invaluable to advancing science.”
Sarah Richardson
“Through my work and being a member of a Diabetes UK Diabetes Research Steering Group, I’ve met and become friends with many people with type 1 diabetes, who remain a huge source of inspiration for me.”
“I see the burden; I see the worry. My goal is to make this burden lighter and one day to hopefully remove it entirely.”
“Conversations with people with lived experience of type 1 are always enlightening, humbling and fuel my determination and passion to make a difference.”
How has your Senior Research Fellowship been progressing so far?
Vicky Salem
“We’ve only just started work on the project, but so far, we’ve recruited the most fantastic group of PhD students and postdocs who come from a range of different scientific backgrounds – biologists, biochemists, material scientists and chemists. Together we’ve already managed to grow blood vessels from cells that have been taken from a patient with type 1 diabetes, giving us a single blood sample.”
“We can extract some cells from that blood sample and grow them in the lab and then use those to build brand new blood vessel networks outside the body. This is the start of the skeleton or the backbone we need to introduce the islets to, to then re-transplant them back into that patient.”
“It’s hugely exciting. We can actually see blood flowing through the blood vessels we’re growing in the lab. This kind of an advance applies not only to people with diabetes, but to all sorts of other regenerative medicine approaches.”
James Cantley
“The fellowship has been really helpful in protecting my time and has given me the ability to focus on research fully.”
“The kudos and publicity surrounding the announcement of the Grand Challenge funding has helped me succeed in recruiting three great people to my team, including a research technician, postdoc and PhD student. Advertising the roles as part of the Grand Challenges attracted high quality international candidates with essential skillsets.”
“I’m very excited to begin the next steps.”
Sarah Richardson
“It’s been very exciting to get started! We’ve recruited some amazing people to our team, the new postdoc and research technician have both really hit the ground running.”
“Together we’ve made a lot of progress, preparing for large-scale imaging analysis and making sure everything is in place for future work. This included upgrading our setup so that up to 10 people can use the software at the same time, both in the lab or remotely. Previously only two people could use it at once and they had to be physically in the lab. This really is a huge step forward!”
“We’ve also collated pancreas images from biobanks around the world, including some very rare samples, allowing us to systematically analyse pancreatic islets in people diagnosed at different ages and stages of type 1 diabetes.”
“We’re also working on getting a few papers submitted to academic journals. The work is fast paced but I’m so grateful to be in this position.”
What is the best thing about your work?
Vicky Salem
“I have the best job in the world. That’s because about 40% of my time is spent with patients, helping them to manage their condition, which is just so rewarding.”
“And of course, talking to patients is incredibly important. There is no point sitting in an ivory tower and coming up with solutions to problems that don’t exist or aren’t important to patients.”
James Cantley
“I’m driven by the excitement of discovering new insights into how the body works, especially the pancreatic beta cell, which has occupied most of my waking hours for the past 20 years.”
“I enjoy the camaraderie and collaborative nature of research, working together towards a common goal, and training the scientists and research leaders of the future. And this Senior Research Fellowship combines all of these!”
Sarah Richardson
“There are less than 700 pancreases available to the research community from people with type 1 diabetes, and even fewer from individuals very close to type 1 diabetes diagnosis where the disease process is most active. Each one looks very different depending on the age someone was diagnosed.”
“One of the best things about my job is spending my day looking at these incredibly beautiful images and working with talented and dedicated researchers to tease out what they can tell us about the root causes of type 1 diabetes.”
Can you tell us about a defining moment in your work as a scientist?
Vicky Salem
“In 2016, I was awarded almost £900,000 of funding from Diabetes UK, to investigate how gut hormones could treat type 2 diabetes and obesity in the future. This was totally life-changing for me because it gave me the opportunity to finish my junior doctor training and become a consultant and at the same time open my own lab and become an independent clinician scientist.”
“At the beginning of this project, I proposed the idea of developing a new way to take images of cells in the pancreas. I remember walking into the room with this huge spinning microscope that cost about £1 million, and thinking, oh my God, where is the on switch?!”
“But even to this day, I remember the first time I saw an image on that microscope of pancreas cells inside a living animal releasing insulin at single cell beta cell resolution, and I thought, yes, I can do this, and I will do this.”
James Cantley
“There have been so many memorable moments in my career, too many to mention! If forced to pick, I would say working on my Diabetes UK-funded PhD project when I was investigating the interaction between oxygen and glucose sensing pathways in beta cells.”
“This was a large project with multiple collaborators, and being involved with so many talented colleagues really underscored the importance of cooperation in science.”
Sarah Richardson
“I will never forget the day I first sat in the lab looking down the microscope reviewing precious donor pancreas tissues, tears streamed down my face as I recognised the loss of so many people, especially children, so far before their time. I want to ensure that we learn from these to improve the lives of those living with type 1 diabetes now and in the future.”
What do you like to do when you’re not working?
Vicky Salem
“I have three children, Georgia is 10, Saul is 11 and Anna is 13, so every bit of spare time I get is focused on them.”
“I have struggled with mum guilt my entire career; I haven’t always been the type of mum that has been at the school gate every day. But I’ve tried to make up for that by talking to them all the time about my work, about the world and encouraging in them the same kind of curiosity that makes my job so fulfilling.”
James Cantley
“When I’m not working, I enjoy spending time with my wife and two daughters, exploring the Scottish Highlands. I’m also a keen climber which helps me to relax and refocus.”
Sarah Richardson
“I have a husband and two daughters, so when I’m not in the lab I take every opportunity to spend time with them and listen to them play music at different open mic nights.”
“I also walk (and run when I can) with my dog, an Australian Kelpie called Mick. Some of my best ideas and solutions to challenges come out of these walks.”
First class research can’t happen without first class researchers, and we couldn’t be more excited to see how the three Senior Research Fellows will break new ground over the next five years.
3. A weekly insulin could be coming
People with type 1 currently take a type of slow-acting insulin, known as basal insulin, once or twice a day to control blood sugar outside of eating. Researchers are developing a new generation of insulins that can work for even longer, reducing the number of injections you need. It may seem counterintuitive, but by editing insulin to make it less effective at clearing glucose, researchers can make it work for longer. This reduced function means it can stay in the body without causing hypoglycaemia.
Novo Nordisk have used this principle to create an insulin called insulin isodec, which has had very promising results in clinical trials. The company has now applied to the US Food and Drug Administration (FDA) for regulatory approval, meaning weekly basal insulin injections could soon become a reality for people with diabetes.
4. Ways to make insulin respond to glucose
Scientists specialising in different disciplines from chemistry to bioengineering have inventive ideas about how to create glucose-responsive insulins, also known as smart insulins. An interesting idea is to create a mixture of insulin and a chemical that can sense glucose, with a large molecule to keep them together.
A team led by Professor Matthew Webber at the University of Notre Dame has developed such a mixture. The insulin mixture is an insoluble blob at a neutral pH, which means not acidic or alkaline. Then, when glucose levels rise, the pH becomes more acidic and the mixture dissolves, releasing the insulin so that it can bind to glucose. Their tests on animals have shown that a single dose of their smart insulin mixture can keep glucose levels stable for up to five days in mice and up to a week in pigs.
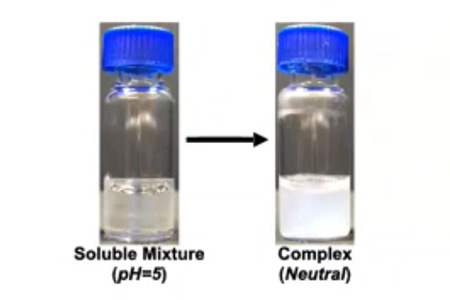
The glucose-responsive insulin mixture in its soluble state and its insoluble state
5. Computer models to streamline research
Treatments must be tested in animals before they can enter clinical trials with people. But lots of drugs that are effective in animals turn out not to work in humans. Professor Michael Strano and his team at MIT have developed a sophisticated computer model of the glucose control system in animals and humans, which can predict how the body will respond to different treatments. The team created the simulation using a combination of maths, biochemistry and extensive data collection from people with type 1.
Researchers can plug their drug designs into the computer model to predict whether it will work or not and edit their designs accordingly. This tool is especially useful for glucose-responsive ‘smart’ insulins because scientists all over the world are experimenting with a range of different approaches to develop them. The simulator will streamline the research process by allowing researchers to only invest time and energy in their ideas that have the best chance of success. It will save crucial time, money and effort in the research and development stage and ensure only the insulins (and other therapies for type 1) with the most potential progress to clinical trials.
Bonus: glucose-responsive glucagon
We can apply all of these ideas for creating glucose-responsive insulin to the hormone glucagon, which has the opposite effect to insulin. Glucagon stimulates glucose production and release from where it is stored in the liver, which is why it is a treatment for severe hypoglycaemia.

A glucagon emergency rescue kit to treat severe hypos
Dr Alborz Madavi, a researcher who founded the company Protomer, believes that a long-acting dose of glucose-responsive glucagon, which could be taken just once a week, would protect against hypoglycaemia. The smart glucagon would turn on at low glucose levels to prevent hypos and work alongside the user’s normal insulin treatment. Dr Mahdavi believes this would help people with type 1 feel less worried about overnight hypos and allow more flexibility with taking insulin.
Type 1 Diabetes Grand Challenge offers hope for novel insulins
The £15 million set aside by the Type 1 Diabetes Grand Challenge to tackle the challenge of novel insulins will expand upon this exciting research to bring these innovative ideas closer to reality. From hormones that can respond to varying glucose levels, to fast- and long-acting insulin, to easier ways to take insulin without injections, novel insulins are coming, and the Grand Challenge will get us there faster.
“Thank you” from a Grand Challenge researcher
May 19, 2023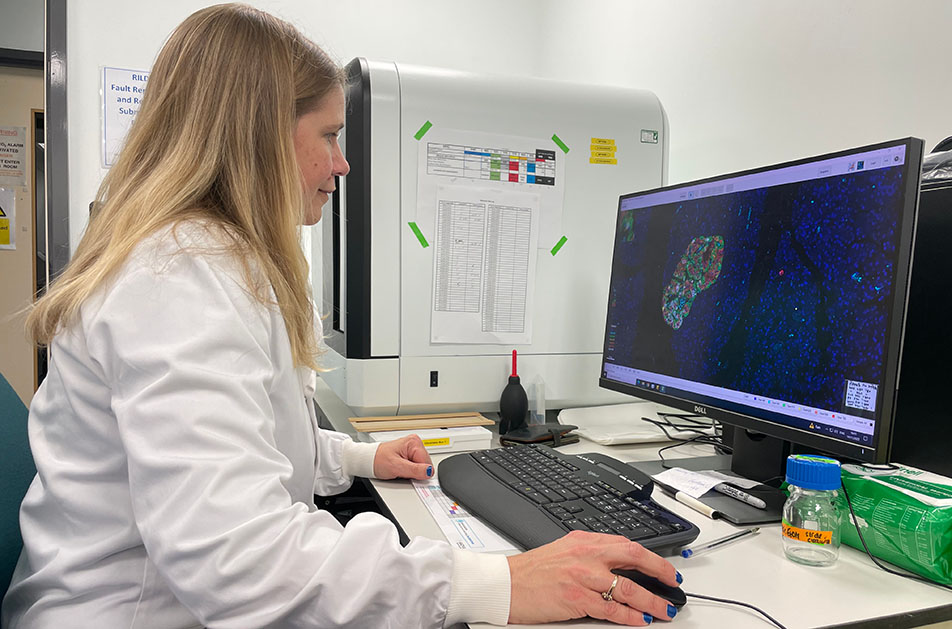
The Type 1 Diabetes Grand Challenge is funding £50 million of research to propel us towards a cure and to change the lives of people living with type 1 diabetes. But the partnership has also been life-changing for the researchers who’ve been awarded Grand Challenge funding.
Earlier this year, Professor Sarah Richardson became one of the first exceptional scientists to receive Type 1 Diabetes Grand Challenge funding.
She’s already made tremendous progress, recruiting staff, setting up her lab, forming collaborations and finalising publications. And she still made time to tell us just what our funding means to her and how the Grand Challenge is building a culture that allows UK type 1 diabetes research to thrive.
“This funding has undoubtedly transformed my research and enthusiasm for life and helped me to build a solid team to push forward our important research.”
“The funds have already made a difference to me, to my team, to UK researchers and most importantly, I know this will ultimately make a difference for people living with type 1 diabetes. Thank you for making this possible.”
Before the fellowship, the demands of her job, gave her little time to focus just on research – but thanks to the Grand Challenge, this has changed beyond recognition.
“There were not enough hours in the day, days in the week and weeks in the year. The pressures were such that I was seriously considering what other options were out there for me. Something I was saddened by as my spark comes alive when I have the opportunity to work in this most important of areas, alongside colleagues who are equally driven and motivated by our common want to change lives for the better.”
“Every day is exciting. We are learning new things, developing new skills – I have learnt how to code – to improve our capacity to deal with large, complex datasets.”
Her team immediately swung into action.
“The team have leapt into the project with curiosity and drive, working carefully and conscientiously to advance our knowledge. I am so proud of how their knowledge and skills are developing, and this supportive environment encourages each of them to push their limits.”
But Sarah and her amazing team haven’t stopped there. Thanks to the Type 1 Diabetes Grand Challenge, they’ve been forging new collaborations with other world-leading teams to help translate what they’ve learned in the lab to people with type 1 diabetes.
“The Grand Challenge calls have got people talking, communicating and networking on a whole other level. The excitement and hope this has generated is palpable, and I am so excited to see the outcomes of this over the coming years.”
______Content of this video______
00:00:00 Introduction to the Novel Insulins Symposium – Professor Simon Heller
00:06:04 Discovery and design of novel insulins – Dr Peter Kurtzhals
00:38:41 Glucose-responsive smart insulin and delivery patch – Professor Zhen Gu
01:09:05 Molecular Engineering of Insulin: Progresses and Challenges – Professor Daniel Chou
01:35:33 Molecular engineering of glucose-responsive insulin – Professor Matthew Webber
02:07:00 Towards oral insulin and an artificial pancreas – Professor Robert Langer
02:26:03 Ultra-stable insulin analogs and their clinical applications – Professor Michael Weiss
02:55:22 Glucose-sensing insulins – Dr Alborz Mahdavi
03:31:42 Diabetes therapeutics from computational design – Professor Michael Strano
03:59:00 Discussion Panel – All speakers
04:36:42 Concluding remarks and next steps – Ms Rachel Connor
“Thank you” from a Grand Challenge researcher
May 17, 2023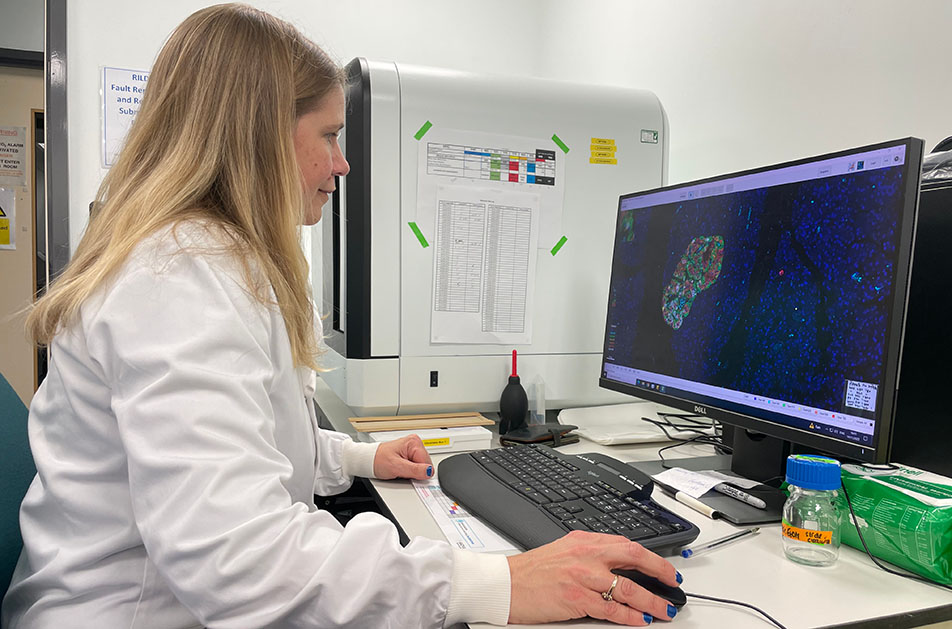
The Type 1 Diabetes Grand Challenge is funding £50 million of research to propel us towards a cure and to change the lives of people living with type 1 diabetes. But the partnership has also been life-changing for the researchers who’ve been awarded Grand Challenge funding.
Earlier this year, Professor Sarah Richardson became one of the first exceptional scientists to receive Type 1 Diabetes Grand Challenge funding.
She’s already made tremendous progress, recruiting staff, setting up her lab, forming collaborations and finalising publications. And she still made time to tell us just what our funding means to her and how the Grand Challenge is building a culture that allows UK type 1 diabetes research to thrive.
“This funding has undoubtedly transformed my research and enthusiasm for life and helped me to build a solid team to push forward our important research.”
“The funds have already made a difference to me, to my team, to UK researchers and most importantly, I know this will ultimately make a difference for people living with type 1 diabetes. Thank you for making this possible.”
Before the fellowship, the demands of her job, gave her little time to focus just on research – but thanks to the Grand Challenge, this has changed beyond recognition.
“There were not enough hours in the day, days in the week and weeks in the year. The pressures were such that I was seriously considering what other options were out there for me. Something I was saddened by as my spark comes alive when I have the opportunity to work in this most important of areas, alongside colleagues who are equally driven and motivated by our common want to change lives for the better.”
“Every day is exciting. We are learning new things, developing new skills – I have learnt how to code – to improve our capacity to deal with large, complex datasets.”
Her team immediately swung into action.
“The team have leapt into the project with curiosity and drive, working carefully and conscientiously to advance our knowledge. I am so proud of how their knowledge and skills are developing, and this supportive environment encourages each of them to push their limits.”
But Sarah and her amazing team haven’t stopped there. Thanks to the Type 1 Diabetes Grand Challenge, they’ve been forging new collaborations with other world-leading teams to help translate what they’ve learned in the lab to people with type 1 diabetes.
“The Grand Challenge calls have got people talking, communicating and networking on a whole other level. The excitement and hope this has generated is palpable, and I am so excited to see the outcomes of this over the coming years.”
“Thank you” from a Grand Challenge researcher
May 11, 2023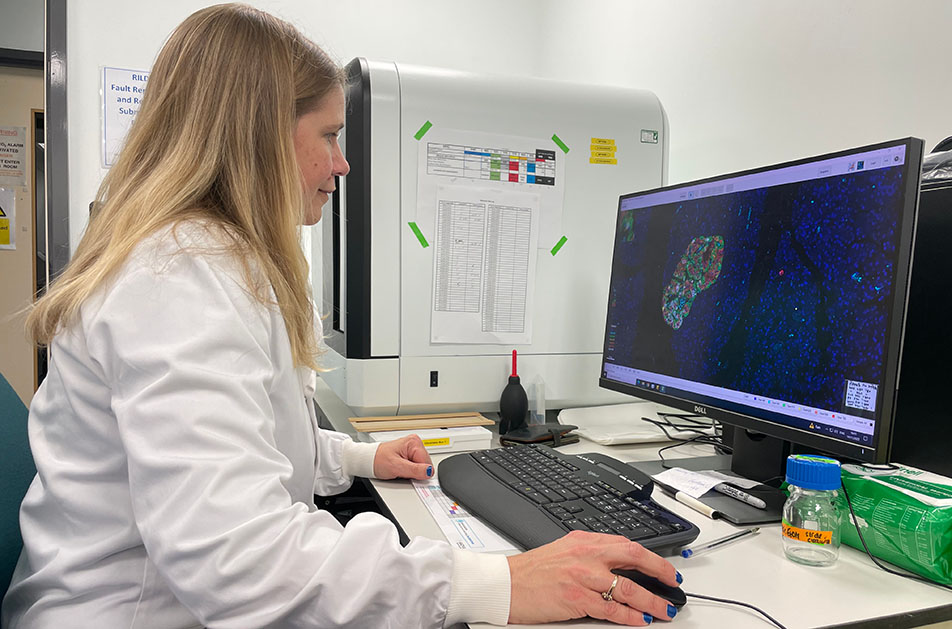
The Type 1 Diabetes Grand Challenge is funding £50 million of research to propel us towards a cure and to change the lives of people living with type 1 diabetes. But the partnership has also been life-changing for the researchers who’ve been awarded Grand Challenge funding.
Earlier this year, Professor Sarah Richardson became one of the first exceptional scientists to receive Type 1 Diabetes Grand Challenge funding.
She’s already made tremendous progress, recruiting staff, setting up her lab, forming collaborations and finalising publications. And she still made time to tell us just what our funding means to her and how the Grand Challenge is building a culture that allows UK type 1 diabetes research to thrive.
“This funding has undoubtedly transformed my research and enthusiasm for life and helped me to build a solid team to push forward our important research.”
“The funds have already made a difference to me, to my team, to UK researchers and most importantly, I know this will ultimately make a difference for people living with type 1 diabetes. Thank you for making this possible.”
Before the fellowship, the demands of her job, gave her little time to focus just on research – but thanks to the Grand Challenge, this has changed beyond recognition.
“There were not enough hours in the day, days in the week and weeks in the year. The pressures were such that I was seriously considering what other options were out there for me. Something I was saddened by as my spark comes alive when I have the opportunity to work in this most important of areas, alongside colleagues who are equally driven and motivated by our common want to change lives for the better.”
“Every day is exciting. We are learning new things, developing new skills – I have learnt how to code – to improve our capacity to deal with large, complex datasets.”
Her team immediately swung into action.
“The team have leapt into the project with curiosity and drive, working carefully and conscientiously to advance our knowledge. I am so proud of how their knowledge and skills are developing, and this supportive environment encourages each of them to push their limits.”
But Sarah and her amazing team haven’t stopped there. Thanks to the Type 1 Diabetes Grand Challenge, they’ve been forging new collaborations with other world-leading teams to help translate what they’ve learned in the lab to people with type 1 diabetes.
“The Grand Challenge calls have got people talking, communicating and networking on a whole other level. The excitement and hope this has generated is palpable, and I am so excited to see the outcomes of this over the coming years.”
“Thank you” from a Grand Challenge researcher
April 27, 2023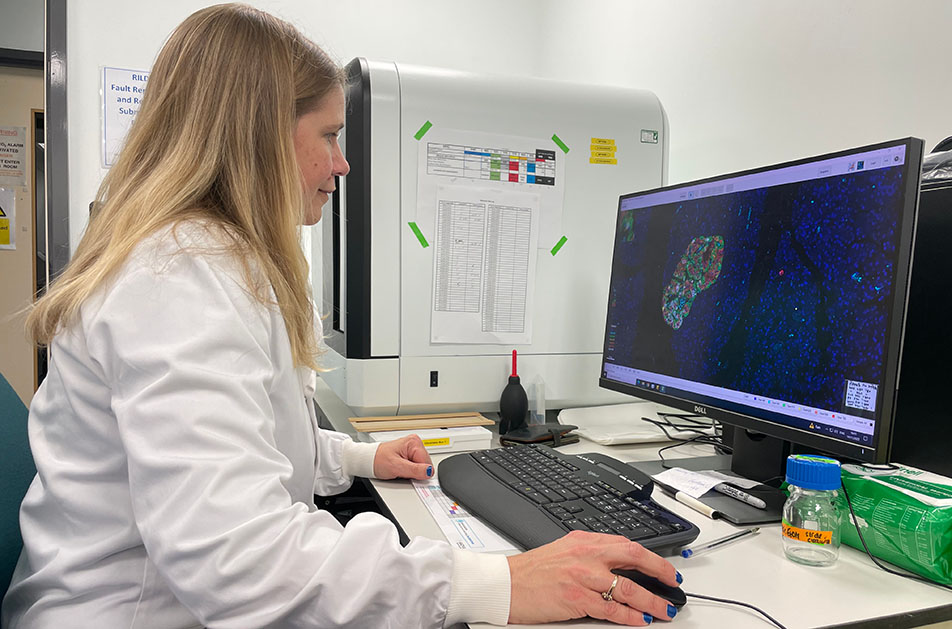
The Type 1 Diabetes Grand Challenge is funding £50 million of research to propel us towards a cure and to change the lives of people living with type 1 diabetes. But the partnership has also been life-changing for the researchers who’ve been awarded Grand Challenge funding.
Earlier this year, Professor Sarah Richardson became one of the first exceptional scientists to receive Type 1 Diabetes Grand Challenge funding.
She’s already made tremendous progress, recruiting staff, setting up her lab, forming collaborations and finalising publications. And she still made time to tell us just what our funding means to her and how the Grand Challenge is building a culture that allows UK type 1 diabetes research to thrive.
“This funding has undoubtedly transformed my research and enthusiasm for life and helped me to build a solid team to push forward our important research.”
“The funds have already made a difference to me, to my team, to UK researchers and most importantly, I know this will ultimately make a difference for people living with type 1 diabetes. Thank you for making this possible.”
Before the fellowship, the demands of her job, gave her little time to focus just on research – but thanks to the Grand Challenge, this has changed beyond recognition.
“There were not enough hours in the day, days in the week and weeks in the year. The pressures were such that I was seriously considering what other options were out there for me. Something I was saddened by as my spark comes alive when I have the opportunity to work in this most important of areas, alongside colleagues who are equally driven and motivated by our common want to change lives for the better.”
“Every day is exciting. We are learning new things, developing new skills – I have learnt how to code – to improve our capacity to deal with large, complex datasets.”
Her team immediately swung into action.
“The team have leapt into the project with curiosity and drive, working carefully and conscientiously to advance our knowledge. I am so proud of how their knowledge and skills are developing, and this supportive environment encourages each of them to push their limits.”
But Sarah and her amazing team haven’t stopped there. Thanks to the Type 1 Diabetes Grand Challenge, they’ve been forging new collaborations with other world-leading teams to help translate what they’ve learned in the lab to people with type 1 diabetes.
“The Grand Challenge calls have got people talking, communicating and networking on a whole other level. The excitement and hope this has generated is palpable, and I am so excited to see the outcomes of this over the coming years.”
You may also be interested in
“Thank you” from a Grand Challenge researcher
April 26, 2023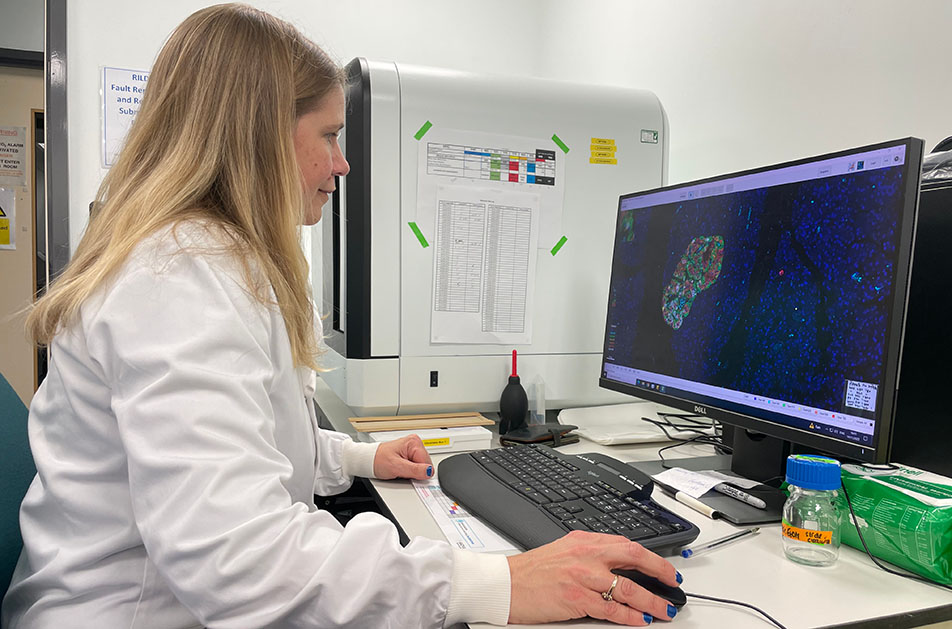
The Type 1 Diabetes Grand Challenge is funding £50 million of research to propel us towards a cure and to change the lives of people living with type 1 diabetes. But the partnership has also been life-changing for the researchers who’ve been awarded Grand Challenge funding.
Earlier this year, Professor Sarah Richardson became one of the first exceptional scientists to receive Type 1 Diabetes Grand Challenge funding.
She’s already made tremendous progress, recruiting staff, setting up her lab, forming collaborations and finalising publications. And she still made time to tell us just what our funding means to her and how the Grand Challenge is building a culture that allows UK type 1 diabetes research to thrive.
“This funding has undoubtedly transformed my research and enthusiasm for life and helped me to build a solid team to push forward our important research.”
“The funds have already made a difference to me, to my team, to UK researchers and most importantly, I know this will ultimately make a difference for people living with type 1 diabetes. Thank you for making this possible.”
Before the fellowship, the demands of her job, gave her little time to focus just on research – but thanks to the Grand Challenge, this has changed beyond recognition.
“There were not enough hours in the day, days in the week and weeks in the year. The pressures were such that I was seriously considering what other options were out there for me. Something I was saddened by as my spark comes alive when I have the opportunity to work in this most important of areas, alongside colleagues who are equally driven and motivated by our common want to change lives for the better.”
“Every day is exciting. We are learning new things, developing new skills – I have learnt how to code – to improve our capacity to deal with large, complex datasets.”
Her team immediately swung into action.
“The team have leapt into the project with curiosity and drive, working carefully and conscientiously to advance our knowledge. I am so proud of how their knowledge and skills are developing, and this supportive environment encourages each of them to push their limits.”
But Sarah and her amazing team haven’t stopped there. Thanks to the Type 1 Diabetes Grand Challenge, they’ve been forging new collaborations with other world-leading teams to help translate what they’ve learned in the lab to people with type 1 diabetes.
“The Grand Challenge calls have got people talking, communicating and networking on a whole other level. The excitement and hope this has generated is palpable, and I am so excited to see the outcomes of this over the coming years.”