Last month, we held a symposium on novel insulins, where experts from around the world met virtually to discuss their ideas for how to develop the next generation of insulins. Their fascinating discussion will be published in a scientific review paper later this year. In the meantime, here is a preview of five of the most exciting ideas that were discussed at the symposium.
1. Fast-acting insulin inspired by snails
We all know how dangerous it is to take too much insulin – and now we’ve found out that even snails understand this. A type of underwater snail called the cone snail uses insulin as a weapon to immobilise their prey. There are subtle differences in this snail’s insulin, which allow it to act much faster than the insulin that people with type 1 currently use. So, diabetes researchers have been teaming up with zoologists to design a super-fast-acting insulin for humans.

A cone snail attacking a fish
Because insulin is such a big molecule, it can take a while to act. Scientists have been trying to make insulin smaller without losing any of its function, but they haven’t been successful yet. Now, researchers including Professor Daniel Chou from Stanford University are trying to mimic the chemical structure of cone snail insulin venom and tweak it slightly to improve its effectiveness in people.
If these researchers manage to create this smaller version of insulin, our skin should be able to absorb it much faster than current insulins. Ultra-fast insulins like this would reduce the time you need to wait between injecting and eating and also offer hope for fully closed loop systems, which don’t require a person to give warning of meals and exercise.
2. Oral insulin pill inspired by tortoises
The problem with taking insulin orally in a pill also partially comes down to its size. If you were to swallow a pill of insulin, it would first break down in your stomach, meaning it couldn’t work properly, and even then, it would still be too big to pass through your intestines. But world-renowned scientist Professor Robert Langer at Massachusetts Institute of Technology (MIT) has developed an ingenious pill that protects insulin and then fires it into the stomach lining.
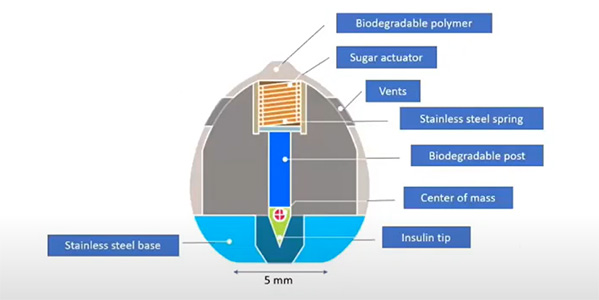
A diagram of Professor Langer’s insulin pill design
The clever design features a tiny spring which propels an arrow of insulin directly into the stomach lining. This happens about an hour after you swallow the device, which is packed inside a biodegradable case, to allow time for it to reach the stomach. But how do you make sure the insulin is always fired into the stomach wall? That’s where the tortoises come in.
A species called the leopard tortoise is self-orienting, which means that it always stays upright. No matter how the tortoise falls or rolls, it will always end up on its feet. This clever trick is due to how its weight is distributed. Inspired by these tortoises, Professor Langer distributed the weight in his insulin pill in the same way so that it always lands with the insulin pointed down.
His pill is called SOMA (self-oriented medical applicator) and Novo Nordisk has so far tested it in 65 people with type 1 diabetes and found no bad side effects.

A leopard tortoise
3. A weekly insulin could be coming
People with type 1 currently take a type of slow-acting insulin, known as basal insulin, once or twice a day to control blood sugar outside of eating. Researchers are developing a new generation of insulins that can work for even longer, reducing the number of injections you need. It may seem counterintuitive, but by editing insulin to make it less effective at clearing glucose, researchers can make it work for longer. This reduced function means it can stay in the body without causing hypoglycaemia.
Novo Nordisk have used this principle to create an insulin called insulin isodec, which has had very promising results in clinical trials. The company has now applied to the US Food and Drug Administration (FDA) for regulatory approval, meaning weekly basal insulin injections could soon become a reality for people with diabetes.
4. Ways to make insulin respond to glucose
Scientists specialising in different disciplines from chemistry to bioengineering have inventive ideas about how to create glucose-responsive insulins, also known as smart insulins. An interesting idea is to create a mixture of insulin and a chemical that can sense glucose, with a large molecule to keep them together.
A team led by Professor Matthew Webber at the University of Notre Dame has developed such a mixture. The insulin mixture is an insoluble blob at a neutral pH, which means not acidic or alkaline. Then, when glucose levels rise, the pH becomes more acidic and the mixture dissolves, releasing the insulin so that it can bind to glucose. Their tests on animals have shown that a single dose of their smart insulin mixture can keep glucose levels stable for up to five days in mice and up to a week in pigs.
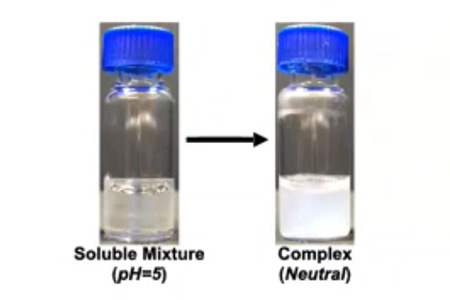
The glucose-responsive insulin mixture in its soluble state and its insoluble state
5. Computer models to streamline research
Treatments must be tested in animals before they can enter clinical trials with people. But lots of drugs that are effective in animals turn out not to work in humans. Professor Michael Strano and his team at MIT have developed a sophisticated computer model of the glucose control system in animals and humans, which can predict how the body will respond to different treatments. The team created the simulation using a combination of maths, biochemistry and extensive data collection from people with type 1.
Researchers can plug their drug designs into the computer model to predict whether it will work or not and edit their designs accordingly. This tool is especially useful for glucose-responsive ‘smart’ insulins because scientists all over the world are experimenting with a range of different approaches to develop them. The simulator will streamline the research process by allowing researchers to only invest time and energy in their ideas that have the best chance of success. It will save crucial time, money and effort in the research and development stage and ensure only the insulins (and other therapies for type 1) with the most potential progress to clinical trials.
Bonus: glucose-responsive glucagon
We can apply all of these ideas for creating glucose-responsive insulin to the hormone glucagon, which has the opposite effect to insulin. Glucagon stimulates glucose production and release from where it is stored in the liver, which is why it is a treatment for severe hypoglycaemia.

A glucagon emergency rescue kit to treat severe hypos
Dr Alborz Madavi, a researcher who founded the company Protomer, believes that a long-acting dose of glucose-responsive glucagon, which could be taken just once a week, would protect against hypoglycaemia. The smart glucagon would turn on at low glucose levels to prevent hypos and work alongside the user’s normal insulin treatment. Dr Mahdavi believes this would help people with type 1 feel less worried about overnight hypos and allow more flexibility with taking insulin.
Type 1 Diabetes Grand Challenge offers hope for novel insulins
The £15 million set aside by the Type 1 Diabetes Grand Challenge to tackle the challenge of novel insulins will expand upon this exciting research to bring these innovative ideas closer to reality. From hormones that can respond to varying glucose levels, to fast- and long-acting insulin, to easier ways to take insulin without injections, novel insulins are coming, and the Grand Challenge will get us there faster.
