Professor Sarah Richardson and her team have made a major breakthrough in understanding why type 1 diabetes is more aggressive in young children, revealing that nearly all their insulin-producing beta cells are destroyed before they can mature. The new insights could pave the way for new strategies to prevent or delay type 1 diabetes and, in time, contribute to a cure.
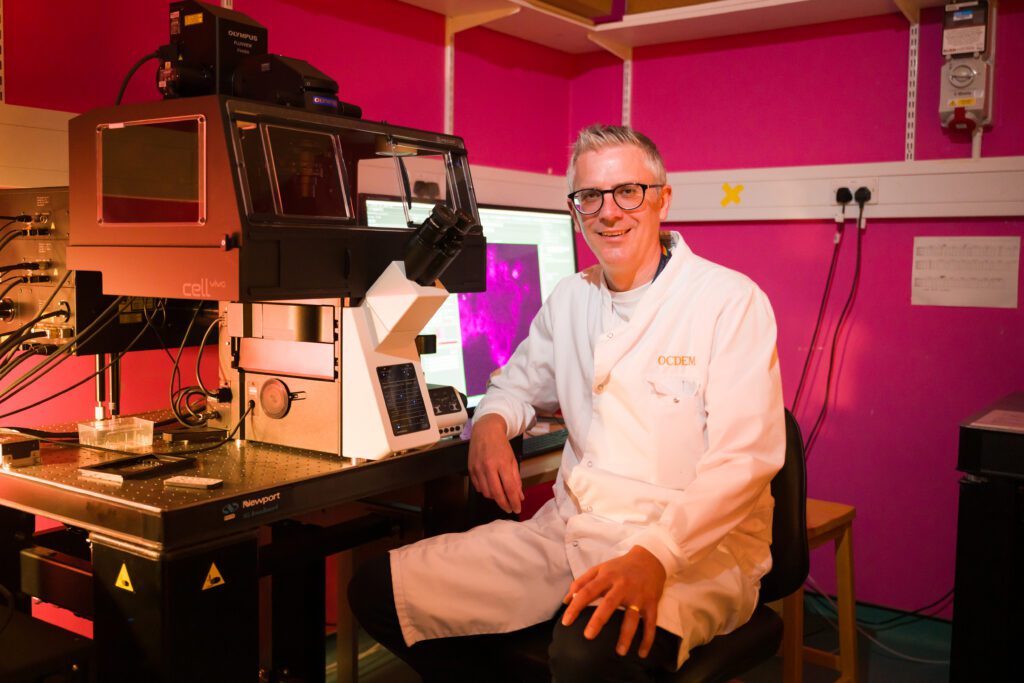
Professor Sarah Richardson, looking at islet samples through a microscope in her lab.
We know that type 1 diabetes is an autoimmune condition, where the immune system attacks and destroys the beta cells in the pancreas. In young children, typically under the age of 7, the immune attack and its destruction of beta cells typically progress rapidly. This can increase the likelihood of diabetic ketoacidosis at diagnosis and make the condition particularly difficult to manage.
Until now, scientists had limited tools to study the early development of beta cells, which are found in clusters in the pancreas. In young children, these clusters are small and still forming, and only contain a few beta cells.
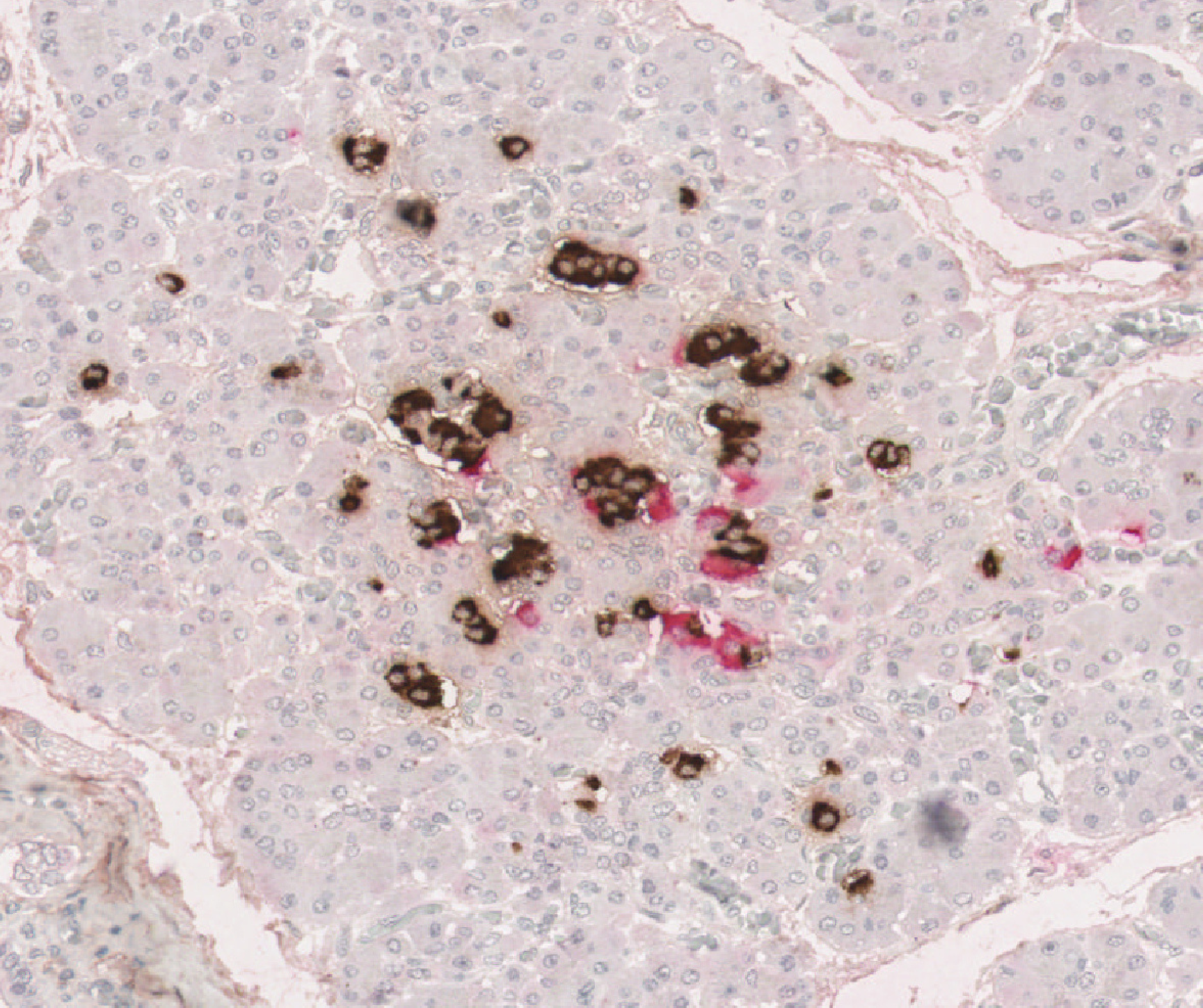
In their latest study published in Science Advances, Professor Richardson and her team used cutting-edge scientific techniques to study these small clusters in unprecedented detail. They analysed rare pancreas samples from over 250 people of varying ages, both with and without type 1 diabetes. They looked at how these clusters change as we age and how they are affected by the immune system.
Teifion Luckett from Sarah’s team, looking at data for their research
The findings confirm that in early childhood, people without type 1 diabetes have many small clusters of beta cells, which normally increase in size and mature with age, with the most rapid development occurring in the first few years of life.
For the first time, our Grand Challenge researchers showed that in people with type 1 diabetes these small clusters are almost completely absent, having been destroyed by the immune system. While some people with type 1 diabetes retained a few large clusters, allowing them to produce small amounts of their own insulin, this was not the case for those diagnosed at a young age.
Together, the results suggest that the abundant small clusters found in young children are especially vulnerable to the type 1 diabetes immune attack. Their rapid destruction prevents them from maturing, leaving very few beta cells later in life. This explains why children diagnosed with type 1 diabetes at a young age typically are unable to produce any of their own insulin, making the condition particularly difficult to manage.
This research underscores the critical role of these small clusters in healthy pancreas development and opens the door for new treatments to protect children’s small clusters of beta cells, giving them the chance to mature into large clusters that are less vulnerable to the immune attack. It also strengthens the case for early type 1 diabetes screening – particularly in young children – essential for identifying those in the early stages of type 1 diabetes before these crucial cells are lost.
Professor Sarah Richardson said:
“These tiny insulin-producing beta cell clusters – once overlooked – hold big clues to understanding type 1 diabetes. This new perspective has the potential to reshape how we screen, treat, and even prevent type 1 diabetes. Protecting small beta cell clusters early could be key to stopping type 1 diabetes before it starts.”
Gareth and Joanne Nye’s daughter was diagnosed with type 1 diabetes at just 23 months old. They told us:
“Gracie’s diagnosis was traumatic for our whole family. In less than 48 hours she went from being a toddler with what we thought was a slight cold, to lying unconscious in a hospital bed with diabetic ketoacidosis (DKA), close to death. We lived in constant fear, setting alarms every two hours to finger prick her at night, worrying if she’d still be with us in the morning.
“Research like this, and the possibilities it holds, will be vital in reducing the number of children diagnosed in critical care, like Gracie. It gives us confidence that one day she could be free from her condition – and that fewer parents and children will have to go through this same experience.”
Dr Elizabeth Robertson, Director of Research and Clinical at Diabetes UK, said:
“The Type 1 Diabetes Grand Challenge set out to fund bold, ambitious research with the potential to fundamentally shift progress toward new treatments and, ultimately, a cure for type 1 diabetes. This study delivers on that vision by challenging the foundations of previous understanding about the development of type 1 diabetes in early childhood.
“Uncovering why type 1 diabetes is so aggressive in young children opens the door to developing new immunotherapies aimed at slowing or stopping the immune attack, potentially giving children more precious years without insulin therapy and, one day, preventing the need for it entirely.”
Rachel Connor, Director of Research Partnerships at Breakthrough T1D, said:
“This study gives us a missing piece of the puzzle, explaining why type 1 diabetes progresses so much faster in children than in adults. For families, that rapid progression can turn everyday life upside down, with a child becoming seriously unwell before the condition is even recognised and parents having to take on a demanding new routine overnight. By revealing how the condition behaves differently in young children, these insights can guide the development of more effective, targeted treatments for young people living with type 1 diabetes.”