Sarah Gatward’s earliest experiences with type 1 diabetes have sparked a lifetime of curiosity and involvement in life-changing research. More than 50 years on, she’s helping others to get involved, to make the Type 1 Diabetes Grand Challenge as impactful as possible for people living with type 1.
Sarah was diagnosed with type 1 diabetes aged 7, after being rushed to hospital, semi-conscious, on 5 March 1972. She was in and out of hospital for a month.
“There were very regimented visiting hours and when the consultant doctors were doing ward rounds parents had to wait outside. The hospital team didn’t want to speak to them.”
Frustrated by this wall of silence, and worried sick about her young daughter, Sarah’s mother urged her to listen carefully to what was being said about her condition, so she could pass it on to her parents and help to look after herself.
“My parents believed very strongly that I needed to understand and be involved with it right from the start. I think it’s helped me enormously.”
A formative experience of research
This early curiosity meant that when an opportunity came up to take part in research into insulin pumps while the family was living in the US, 15-year-old Sarah was keen.
“I’d hit adolescence and everything changed enormously. I was having bad hypoglycaemia overnight which would lead to nighttime convulsions. There was no easy way of trying to work out what was causing it and how [my doctors] should manage it”
Sarah joined a one-year research trial, which showed that insulin pumps achieved better blood sugar management than three insulin injections per day in young people. This was an important finding for the future of type 1 treatment and had a life-changing influence on how Sarah managed her condition.
“Taking part in the pump research provided me with the means to adjust my treatment to suit my day-to-day life. Until that point, I’d had quarterly hospital reviews where dose adjustments were made before I was sent home to continue with that fixed pattern for the next three months. I had learned it worked better to flex my treatment according to daily needs, and the pump allowed me to do that.”
Getting involved
That first encounter with research was just the start. Over the years Sarah has participated in other clinical trials looking at different aspects of type 1 management, before getting involved as a patient adviser.
“Breakthrough T1D were looking for a group to review and approve small grant award applications. It was made up of healthcare professionals, researchers and patients. I brought my experience of life with type 1 and professionals brought their knowledge of the condition and we worked together. I sat on the committee for four years and it was a really positive experience.”
Lived experience in the Grand Challenge
During her time on the Scientific Advisory Board, Sarah got to know several researchers working in the field. This led to her being invited by Professor Shanta Persaud and Professor Aileen King to assist with an application for an ambitious research application to the Grand Challenge.
Their beta cell therapy programme was funded, and Sarah now leads a group of people with lived experience of type 1 who work with the research team. This is commonly known as Patient and Public Involvement (PPI) and—as Professor King explains—the Grand Challenge ensures PPI isn’t just a box-ticking exercise.
“We have really benefited from having Sarah as a co-applicant on our grant. While we’ve engaged with patients in the past, it was never as structured or sustained as it has been through the Grand Challenge. With Sarah, we’ve built a PPI group that we’re really proud of. We hold regular meetings and are planning the group’s second visit to our labs. It’s been a privilege to get to know them.”
The PPI group brings valuable first-hand insights from people of different ages and experiences. For instance, two members have had islet cell transplantation. They shared their insights in a session for the researchers, who are considering the practicalities of delivering stem cell-derived beta cells to people with type 1 diabetes.
Professor King continues:
“It was really eye-opening for us. Although we were aware of the scientific practicalities of the procedure, it brought to light the process from a patient point of view. We gained a deeper understanding of what it’s truly like to wait for a transplant, and the significant sacrifices patients often have to make afterwards.
“I think the whole team felt really inspired. Sometimes science is hard and bringing extra inspiration to our team to remind them why they are doing these difficult experiments is important. These insights [also] remind us to stay mindful of what patients actually want to achieve. It helps guide our research to remain aligned with their needs and expectations.”

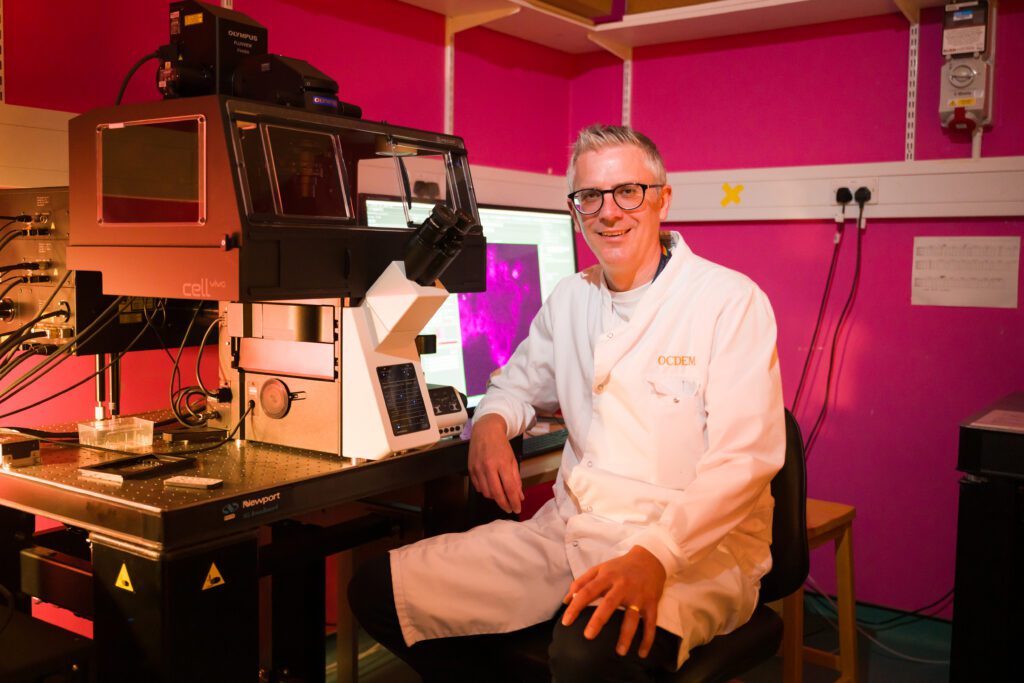
Researchers at King’s College London with their Patient and Public Involvement members
Optimism and hope
Sarah describes herself as a ‘realistic optimist’; believing that research can improve things but knowing that it can take time. This outlook has been shaped by the incredible advances in type 1 treatment she’s experience over the decades, which were unimaginable to her as a child.
“I had the kit I needed for urine testing in our downstairs toilet and it was all quite squished balancing the equipment around the edge of the wash basin. I remember fantasising that when I’m an adult I’m going to have a special room that I can have all my medical kit in so that I could spread it out and have space around me. It just never occurred to me that I would no longer be undertaking urine tests and that the equipment available for managing the condition would be so much more advanced!”
Now, with the Grand Challenge, Sarah’s sights are set on a day when she doesn’t have to be injecting insulin at all.
“We’re getting closer and closer. I’ve talked about it with a couple of friends who have also been living with type 1 long term and we’ve often joked about what on earth we would do with all the spare mental capacity that a cure would bring! It would be absolutely wonderful to have that headspace back, having a life where I don’t have to think about type 1 all the time.”