Home »

This article is written by Dr Craig Beall and is republished from The Conversation under a Creative Commons license. Read the original article.
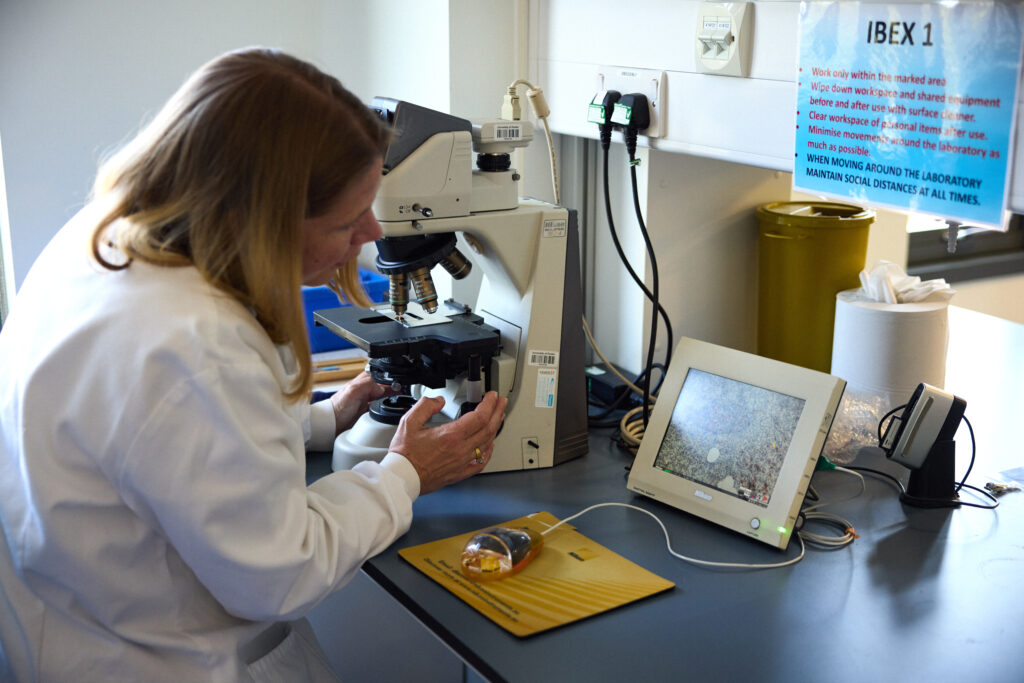
Dr Craig Beall in his research lab
Your brain makes insulin – the same insulin produced by your pancreas. The same insulin that is not produced in people with type 1 diabetes and the same insulin that does not work properly in people with type 2 diabetes.
Scientists have known for over 100 years about insulin producing cells in the pancreas. These spherical islands of cells, called islets, contain insulin producing beta cells.
But we’ve only just started to learn about brain insulin production. The fact that insulin is made there is still largely unknown, even among diabetes scientists, doctors and people with diabetes.
Yet, it was discovered there in the late 1970s – then promptly disregarded.
A study published in 1978 showed the levels of insulin in the rat brain were “at least 10 times higher than that found in plasma … and in some regions … 100 times higher”. If true, why isn’t this more widely known.
Because soon after this discovery, clear evidence showed the transfer of insulin from blood to brain. One study in 1983 measuring insulin in rodent brain said that “insulin found in these extracts was ultimately derived from pancreatic insulin”. They could not find the machinery to process insulin in the brain, at least with the tools available at the time.
This led to the assumption – for nearly the next 30 years – that all brain insulin came from the pancreas.
Insulin can and does move from the blood to the brain. But local sources of insulin are produced in specific places to do specific things.
The brain cells that make insulin
First, what is surprising about brain insulin production is that there is not one but at least six types of insulin-producing brain cell. Some have been confirmed in both rodent and human brain, others currently just in rodents.
One of the first brain cells shown to make insulin is the neurogliaform cell. These live in a brain area important for learning and memory. Most surprisingly, the production of insulin here depends on the amount of glucose present – a feature shared with pancreatic beta cells.
Its not clear what this insulin source does. Based on the location, it may contribute to cognitive function.
This area also has cells that create new neurons throughout life, called “neural progenitors”. These cells also make insulin.
A similar cell from the olfactory bulb, the processing centre for smell, also has insulin-producing progenitors. What insulin does here is still unknown.
But one insulin producing brain cell might regulate growth. A 2020 study showed that insulin is made and released from stress-sensing neurons in the mouse hypothalamus. This is a brain area that controls growth and metabolism. It also has the highest insulin levels in the human brain.
The researchers showed that stressing mice caused hypothalamic insulin production to decrease. This led to poorer growth in the animals. In the case of mice, their bodies were shorter.
Hypothalamic insulin maintained growth hormone levels in the pituitary gland. This is sometimes called the master gland as its involved in making or controlling production of other hormones. Having less local insulin meant less growth hormone production.
Then there is the choroid plexus. This is the brain region that makes cerebrospinal fluid. In humans, that is about half a litre of this clear colourless liquid every day.
Cells lining the choroid plexus – the epithelial cells – make a nourishing broth of growth factors and nutrients to keep the brain healthy. Only recently was insulin production found here in mice.
The choroid plexus secretes fluid directly into brain ventricles, the spaces deep inside the brain. This fluid flows around the whole brain, perhaps delivering insulin more widely.
One place it does travel to is the appetite control centre in the hypothalamus.
A 2023 study in mice showed that genetic control of insulin production by the choroid plexus could change food intake. The hypothalamus was rewired by changing choroid plexus insulin levels. Insulin released from here suppressed appetite.
Another source of insulin in the brain also reduces food intake. A 2022 found that insulin producing neurons at the back of the brain, called the hindbrain, reduced food intake in mice.
Might help the brain stay healthy as we age
So if brain insulin can change appetite, does it control blood sugar?
No. At least there is no evidence for this currently. It is unlikely this insulin leaves the brain. Therefore, its unlikely to control glucose levels in the same way.
Instead, insulin in the brain might help the brain stay healthy as we age. For example, Alzheimer’s disease is often, unofficially, termed type 3 diabetes. This is because the brain is insulin resistant in Alzheimer’s. It cannot properly use glucose either.
This is a big problem. Glucose is the main fuel for the brain. In fact, estimates suggest there is a 20% energy gap in Alzheimer’s. Even without brain cell loss, this alone will impair cognitive performance.
This has led to attempts to boost brain insulin. Spraying insulin into the nose can improve cognitive performance in Alzheimer’s, in some, but not all studies.
Brain glucose use also decreases over time and intranasal insulin also seems to limit this decrease.
Therefore, is more brain insulin always a good thing?
Not necessarily. In women specifically, higher levels of insulin in cerebrospinal fluid is associated with poorer cognitive performance.
There is still much to learn about brain insulin production. For example, which insulin source came first? The brain or the beta cell? Hopefully it doesn’t take another 30 years to find out.
But given the strength of evidence of brain insulin production, it won’t be long until our school textbooks are updated.
Read more about the Type 1 Diabetes Grand Challenge project led by Dr Craig Beall and Dr Thomas Piers that looks at how to make use of brain insulin production to improve beta cell therapies.
Viral triggers, ticks to tackle the immune system and a smart coat for insulin: Latest type 1 diabetes research
May 27, 2025
At the Type 1 Diabetes Grand Challenge, we support cutting-edge research aimed at bringing us closer to better treatments, and potentially, a cure. The research teams we fund are leaders in the field and their latest discoveries, highlighted here, are contributing to global efforts to transform the treatment of type 1 diabetes.
Connection between a common virus and type 1 diabetes
The development of type 1 diabetes is caused by a complex interplay of genetic and environmental factors, which trigger the immune system to turn on and destroy insulin-producing beta cells. The Type 1 Diabetes Grand Challenge is investing in research to learn more about precisely what goes wrong and how this process unfolds.
An international research team, including our Senior Research Fellow Professor Sarah Richardson, has just published the strongest evidence to date that enteroviruses play a role in the development of type 1 diabetes.
They studied pancreas samples from nearly 200 donors to check for signs of enterovirus infections. These included samples from people with and without type 1 diabetes, as well as individuals who had type 1 diabetes autoantibodies – early immune warning signals that indicate a high risk of developing the condition in the future.
They reported that signs of enterovirus infection were most common in people with type 1 diabetes who still had some functioning beta cells. Infections were also present in people with autoantibodies, but much less common in those without diabetes or in people with type 1 whose beta cells had already been completely destroyed.
A key finding was the presence of a protein made by the enterovirus, called VP1. The researchers found VP1 was strongly linked to high levels of HLA class I molecules. These are markers of an early immune system response in the pancreas. This is the first time these viral and immune markers have been found together – including in the early stages of type 1 before a diagnosis.
These findings offer the strongest evidence to date that enteroviruses may trigger or accelerate the onset of beta cell destruction in early type 1 diabetes. A clearer understanding of their role could lead to new approaches that target the immune processes they influence — potentially slowing or even preventing type 1.
‘Ticking’ beta cell protection
One part of a solution to curing type 1 diabetes is to transplant beta cells, either donated or grown in labs, into people with type 1 so they could produce their own insulin again. However, the immune system is primed to attack the new cells too. This happens partly because the transplanted cells release chemokines—chemical signals that attract immune cells. Blocking these signals is difficult, as there are many different types.
Scientists have discovered that ticks produce proteins called evasins that can block several of these signals at once. Professor Shoumo Bhattacharya’s team has studied these evasin proteins and identified the specific peptides that have this powerful blocking ability. They’ve established a new method that allows them to test many versions of these peptides rapidly, and pinpointed those that work best at calming the immune response.
Published in Communications Biology, these innovative findings lay the groundwork for Professors Shoumo Bhattacharya and David Hodson’s Grand Challenge project. They aim to use these peptides to help protect new beta cells from immune attack after being transplanted. This could create a safer alternative to immunosuppressive drugs and improve the success of beta cell therapies for type 1 diabetes.
Giving insulin a smart coat
Professor Zhen Gu’s team at Zhejiang University in China has developed a new insulin delivery system, called i-crystal, as reported in their latest publication in Nature Nanotechnology.
Designed to help people with type 1 diabetes keep blood sugar levels within target range, the system uses specially coated insulin crystals that release insulin slowly and steadily. The coating is a unique membrane that enables the crystals to respond precisely to changes in blood sugar and ketone levels. This means insulin is only released when blood sugar levels rise and stops when it drops, helping people with type 1 avoid highs (hypers) and lows (hypos).
Early tests show that i-crystal could help regulate blood sugar levels for over a month in mice after just one injection, and for more than three weeks in minipigs after five daily doses. This suggests this delivery system could reduce the need for frequent injections and make daily diabetes management easier.
If successful, i-crystal could offer a safer, longer-lasting, and more adaptable form of insulin therapy for people living with type 1 diabetes.
What are beta cell therapies, and do they offer hope for a cure for type 1 diabetes?
April 15, 2025
Clinical trials in beta cell replacement are creating a buzz among the diabetes community. We explain what beta cell therapies are, how close they could be to becoming a potential treatment option, and how Grand Challenge research is helping bring them closer to the reality.
In type 1 diabetes, the immune system attacks the beta cells in the pancreas, which make insulin. Insulin is essential for regulating our blood sugar levels. So people with type 1 have to check blood sugar and take insulin multiple times a day, every day, to stay alive.
For many people, the advances in diabetes technologies mean that some of this constant checking and dosing can now be done automatically by continuous glucose monitoring and hybrid closed loop systems. However, even the latest tech cannot get close to mimicking the body’s finely tuned system for keeping glucose in check.
One of the most promising routes to a cure for type 1 diabetes is to seek ways to replace the lost beta cells and restore insulin production. We know it can work – the first successful human transplants of beta cells taken from a donor happened as far back as 1990.
The parts of the pancreas that contain beta cells are known as islets. In 2008, the UK launched an islet transplant programme for people with type 1 diabetes who experience frequent life-threatening episodes of low blood sugars (severe hypoglycaemia, or ‘hypos’) but have no awareness of the warning signs. It was an exciting advance, offering the hope of freedom from insulin therapy for some.
Islet transplants are limited
While islet transplants are pretty effective at giving people more stable blood sugar levels and cutting episodes of dangerous lows, there are several reasons why they’re not widely suitable as a treatment for type 1:
- Data suggests that an average of 3 donor pancreases are needed for 1 successful transplant. Donor organs are sourced from deceased individuals and – like most transplant programmes – the demand severely outweighs the supply of usable tissue.
- Transplants from a donor may be rejected by the body, so recipients must take lifelong medication to suppress their immune system (immunosuppressants). This leaves people compromised – at greater risk of certain cancers and severe infections.
- Despite immunosuppression, transplanted islets often fail to survive in the long term because they can’t get the oxygen and nutrients they need.
- While they can allow some people to temporarily stop insulin therapy, this is rarely permanent. Over time, most people will need insulin again, although usually at lower doses.
Fewer than 350 islet cell transplants took place in the UK between 2008 and 2022. There’s an urgent need to find effective and sustainable alternative approaches to beta cell replacement that can be accessed by many more people with type 1. That’s why beta cell replacement is one of the three major research themes of the Type 1 Diabetes Grand Challenge.
Exciting trials underway
Some of the most talked-about research happening in type 1 diabetes right now are clinical trials in beta cell replacement.
One trial, led by a company called Vertex, is testing transplants of beta cells grown in the lab. The results have been really promising, with some participants no longer needing insulin. However, they still need powerful immunosuppressants to prevent rejection. The treatment is now in the final phase of testing, and if all goes well, Vertex plans to seek global approval in 2026. It’s likely this would initially only be for people who experience frequent severe hypos and have no hypo awareness.
In October 2024, Chinese researchers reported positive results using beta cells grown from a patient’s own stem cells. It’s very early days – they only tested it in one person – but this approach has potential to overcome the rejection problem because the transplanted cells would be recognised as ‘self’.
Another first-in-human study was reported by Sana Biotechnology at the start of 2025. They used donor beta cells but gene-edited them to become invisible to the immune system. After four weeks the transplanted cells had avoided immune attack and were producing insulin.
The bigger picture
Type 1 diabetes is complex and we’re unlikely to land on a one-size-fits-all cure. So, while the current trials are hotly anticipated, they’re only one part of the story. And that’s why the Type 1 Diabetes Grand Challenge is funding over £16 million into 10 research projects looking at building better beta cells for transplantation, protecting beta cells during and after transplantation and regrowing beta cells in people with type 1 diabetes.
Nearly two decades after the islet transplant programme launched in the UK, we’re getting closer to better beta cell replacement therapies. And the Grand Challenge is helping to push the pace of progress so that more people can be released from the daily burden and dangerous complications of type 1 diabetes.
You may also be interested in
The Type 1 Diabetes Grand Challenge makes waves at DUKPC
The Type 1 Diabetes Grand Challenge took centre stage at this year’s Diabetes UK Professional Conference, uniting researchers and people affected by type 1 diabetes to share their expertise and celebrate progress with the wider diabetes community.
March 14, 2025
The Type 1 Diabetes Grand Challenge took centre stage at this year’s Diabetes UK Professional Conference, uniting researchers and people affected by type 1 diabetes to share their expertise and celebrate progress with the wider diabetes community.
Our community in the spotlight
The main Grand Challenge session was a powerful showcase of our ever-growing community, featuring 13 new projects we’ve funded in the last year.
The session began with updates from researchers working to build better beta cells in the lab from stem cells, protect new cells during and after transplantation, and regrow beta cells in people with type 1 diabetes.
Later on in the conference, we heard more about islet transplantation, using cells from donor pancreases. Prof Shareen Forbes discussed the potential of microparticle drug delivery to protect transplanted islets and improve their survival. And we were joined by Dr Vicky Salem who highlighted innovations in biomaterials that could transform islet transplantation.
Our immune insights project leads shared exciting progress on targeting the type 1 immune system attack in safer and more effective ways. Dr James Pearson revealed that some immune cells follow a daily rhythm, and that’s why his project is testing if immunotherapies timed to these cycles will improve their effectiveness.
We also welcomed Profs Michael Weiss, Matthew Webber and Zhiqiang Cao, who discussed their eye-opening ideas to develop novel insulins that could act more quickly and precisely, ultimately reducing the burden of type 1 diabetes management.

Picture of Profs Michael Weiss, Matthew Webber accepting their awards; credit: © Julie Broadfoot
You can find more details about each project presented at DUKPC on our funded projects page.
Lived experience at the heart of research
A dedicated session at DUKPC highlighted how the quality and impact of Grand Challenge research is being enhanced by meaningfully involving people with lived experience of type 1.
Heather Robinson, a Together Type 1 young leader, shared striking statistics on the difficulties of transitioning from paediatric to adult diabetes care, underscoring the need for greater involvement from those directly affected.
Dr James Pearson echoed this, sharing how the challenge of recruiting young adults with type 1 for research led him to involve them more actively through the Cardiff Diabetes Innovation Committee. Committee members reflected on how this engagement deepened their understanding of type 1 diabetes and ensured research truly benefits those who need it most.

Picture of Dr James Pearson and Lilly from the Cardiff Diabetes Innovation Committe; credit: © Philippa Gedge Photography
Recognising the importance of lived experience in research, Professor Sean Dinneen spoke about working with young adults with type 1 to identify gaps in care and improve treatments, while Dr O’Donnell showcased his project co-developing user-led technology that prioritises real-life experiences and emotional well-being.
Amelia Burke, a glass artist from Wales and mum of Ruby who lives with type 1, emphasised that involvement must be accessible and approachable. Her interactions with Grand Challenge researchers inspired her to use artistic methods to represent her daughter’s experience and raise awareness about beta cell therapies.
Heather shared her experience at the conference with us:
“Getting to experience DUKPC from multiple perspectives was such a unique and unforgettable opportunity. From interviewing researchers, speaking on a panel, meeting other Young Leaders from the Together Type 1 program and presenting in the Grand Challenge Patient and Public Involvement session, it was a jam-packed few days! Being able to watch the involvement of experts by experience increase over the past few years has been brilliant, and with the collaboration of Steve Morgan Foundation, Diabetes UK and Breakthrough T1D has only developed this. Speaking with researchers and experts by experience brought such a broad range of viewpoints and I’m so excited for the future of patient-led diabetes research and healthcare.”

Picture of Heather with Dr Craig Beall at DUKPC
Bringing research to reality
For research to truly make an impact, scientific breakthroughs must be translated into real-world solutions. And that’s exactly what we’re aiming to achieve through the Grand Challenge— accelerating great ideas to change the lives of those affected by type 1 diabetes. As part of this, we hosted a ‘Top Tips on Commercialisation’ session, bringing together experts in research funding, policy, and entrepreneurship to share practical advice on turning research into real-world impact. This is just the beginning —throughout this year we’ll continue to support our community in in moving innovations from the lab into people’s lives.
Dr Andy Chapman, CEO and Co-Founder of Carbometrics says:
“Thank you to Type 1 Diabetes Grand Challenge for inviting me to speak at the Diabetes UK Professional Conference 2025 in Glasgow. It was a privilege to join such an esteemed panel to discuss the challenges and future of commercialisation in diabetes technology, and connect with fellow innovators in this space.”
Dr Bethany Cragoe, Charity Business Manager of LifeArc, says:
“Charities are crucial in getting research to patients by leveraging the expertise of many stakeholders including patients, scientists, clinicians, and industry partners. Technology transfer is key in this process, and early engagement with technology transfer offices helps develop effective intellectual property strategies and potential routes to patient benefit.
“Researchers should understand the translational pathway and plan early to ensure their work benefits patients. Building strong networks with industry and funders is key to success in this journey. Organisations and initiatives such as Knowledge Exchange UK, Innovate UK and Association of Technology Transfer Professionals can support this. All these elements must come together to ensure that the funded research outputs are able to realise their maximum potential for patient benefit.”

Picture of Dr Bethany Cragoe speaking at the ‘Top Tips on Commercialisation’ credit: © Philippa Gedge Photography
New funding available to boost beta cell research in the UK
December 20, 2024
We’re launching a new funding call to address the limited availability of stem cell-derived beta cells for research purposes.
The aim is to facilitate more high-quality research into beta cell therapies, speeding up progress towards a cure for type 1 diabetes.
To achieve this, we’ve partnered with the Advanced Regenerative Manufacturing Institute (ARMI), the US leading organisation in manufacturing cells, tissues and organs.
Funding is available for UK-based researchers to test if stem cell-derived beta cells produced by ARMI can survive shipment from the US to the UK. And if they can, whether they work as expected in both lab studies and living organisms.
We’re inviting UK experts with a track record of producing and testing stem cell-derived beta cells to apply for funding to test ARMI’s beta cells. Funding is available for up to three sites across the UK.
Successful researchers will also have the opportunity to directly compare ARMI’s beta cells with their own lab-made beta cells. This may help them to improve their own production process and identify the most effective product for wider rollout.
The hope is that it will enable the development of a reliable supply of high-quality, pre-made stem cell-derived beta cells for use by UK scientists. By saving researchers time and ensuring consistency across studies, this initiative is expected to accelerate the development of new beta cell replacement therapies.
Apply for funding
Details about the call can be found here. You’ll need to submit your application by 31 January 2025.
If you’re interested in applying, we strongly encourage you to attend our funding call webinar on 8 January 2025 at 14:00 GMT and reach out to the T1DGC Research Funding Team to discuss the opportunity further (smfgrandchallenge@diabetes.org.uk).
The Advanced Regenerative Manufacturing Institute (ARMI | BioFabUSA) said:
“ARMI is proud to partner with the Type 1 Diabetes Grand Challenge to advance beta cell research. By providing high-quality, stem cell-derived beta cells for validation, we aim to accelerate breakthroughs in type 1 diabetes treatment and improve the scalability of regenerative therapies. This initiative represents a critical step in bridging global efforts to bring innovative solutions to patients.”
Professor Matthias Hebrok, Vice Chair of the Type 1 Diabetes Grand Challenge Scientific Advisory Panel, said:
“Testing stem cell derived islets produced by a foundry for their functional properties upon being sent to the UK is critical to ensure high quality tissues will be available to accelerate research in type 1 diabetes.”
Funding call: Stem Cell Derived Beta Cell Product Validation Sites

Funding call: Stem Cell Derived Beta Cell Product Validation Sites
Amount: Up to three grants available with the total for each site determined by the costs required by each Host Institution to deliver the work described.
Duration: ~12-months for the validation study with work likely commencing from the end of May 2025 subject to cell production and shipping arrangements.
Skills: Independent group leaders with teams who have a track record of working with and/or producing stem cell derived beta cells and studying them both in vitro and in vivo.
Location: Will fund up to three validation sites. The Principal Applicant at each location must be based at an academic Host Institution in the UK. Applications led by or including commercial organisations will be considered on a case by case basis.
Process: Short application submitted through the online grant’s portal, accompanied by a full financial breakdown, by 31 January 2025.
Purpose: To test and validate stem cell derived beta cell products manufactured by the Advanced Regenerative Manufacturing Institute (ARMI). Applicants may propose additional, related project tasks (e.g., the inclusion of additional stem cell derived beta cell sources for comparison).
There is a need to address the limited availability of stem cell derived beta cells for academic research studies. To achieve this at pace we have partnered with the Advanced Regenerative Manufacturing Institute (ARMI), based in New Hampshire, US. ARMI focuses on the scalable, consistent, cost-effective manufacture of cell-based products. Scaled manufacture will enable a reliable supply of stem cell derived beta cells to researchers, and the three original validation sites will be prioritised for consideration as major distribution hubs.
If you’re interested in applying, you can refer to some frequently asked questions here, or watch the below webinar recording and hear from Diabetes UK and ARMI teams, who have given more contexts to this funding call and some top tips for making a stand out application. Or you may refer to some frequently asked questions here.
Scope
The validation study is designed to determine cell viability in shipping from the US to the UK, as well as cell function both in vitro and in vivo. Flexibility on receipt and testing days will be needed due to the unknowns that can occur with international shipments. As above, applicants may propose additional, related project tasks (e.g., the inclusion of additional stem cell derived beta cell sources for comparison). To note, the three sites will need to use standard procedures to ensure the results are comparable and therefore, will be required to collaborate if successful. The same transplant procedure will also ideally be adopted at all three locations.
We are also open to applicants pitching to add a third comparator to the study, if they also have a proven protocol used in their laboratories to produce stem cell derived beta cells and test in vitro and in vivo. All results generated must be shared back with ARMI and each site will use aligned collection and reporting templates/platforms.
Scope of Work for the Stem Cell Derived Beta Cell Validation Study
The Scope of Work (SOW) includes the ability to:
- Receive stem cell derived beta cells and maintain in culture until in vitro and in vivo assessment is performed;
- Perform in vitro assays to assess stem cell derived beta cell morphologically, compositionally (e.g. by flow cytometry) and functionally (e.g. glucose-stimulated insulin secretion assay);
- Perform 12-week in vivo assessment of the stem cell derived beta cells by implanting under the kidney capsule of a suitable mouse model of diabetes (e.g. streptozotocin-induction in an immunodeficient background) and assess by using the appropriate tests (e.g., blood glucose measurement, animal weight, human c-peptide, periodic intraperitoneal glucose tolerance test);
- And perform histology on explanted grafts to assess graft durability.
Eligibility criteria
This call is open to non-clinical and clinical independent group leaders based at academic Host Institutions within the UK. Applications led by or including commercial organisations will be accepted and considered on a case by case basis, and we encourage you to contact the T1DGC Research Funding Team to discuss your application. Applications must be led by one Principal Applicant but can include other experts from their or other Host Institutions as Co-Applicants/Collaborators plus project management/co-ordinator support. As we will fund up to three sites that will be required to collaborate if successful, we are open to receiving applications that are interlinked from the start. But separate submissions will still be required.
Skills and expertise
In addition to experience of working with and/or producing and testing stem cell derived beta cells, the appropriate Home Office approvals should be in place, or able to be, by the earliest start date of 31 May 2025, to conduct the animal studies described.
Assessment criteria
Applications will be scientifically assessed by a subset of the Beta Cell Therapy Reviewer college, a group of international beta cell experts, and co-opted experts where necessary. The reviewers will focus on:
- Relevant experience, skills, and expertise in beta cell therapy research.
- The research environment and personnel, and the ability to conduct and deliver the experiments as described in the SOW provided as part of the funding call, within the timeframe described.
- Ambition to help address this barrier to progress, the availability of stem cell derived beta cells for research purposes.
The recommendation from the Scientific Review Panel will be considered by ARMI, the Beta Cell Therapy Scientific Advisory Panel, who provide strategic guidance to the partnership, and the Type 1 Diabetes Grand Challenge Partnership Steering Group, composed of representatives from the three partner organisations Diabetes UK, the Steve Morgan Foundation and Breakthrough T1D UK.
Guidelines and Terms and Conditions
General Guidelines for Research Grant Applicants
Steve Morgan Foundation Type 1 Diabetes Grand Challenge Grant Conditions
A Material Transfer Agreement (MTA) will need to be signed for applicants to receive and test the cells. As this is a validation study using cells provided by ARMI some of the specific grant conditions for work funded by the Type 1 Diabetes Grand Challenge will not be relevant. For any work carried out on other cells sources, the standard terms apply.
Funding
Financial leverage is essential to the T1DGC initiative as we can do more together. Therefore, we ask that Applicants discuss this opportunity with their Host Institutions and explore how we can work in partnership, such as covering indirect costs and making contributions to the direct costs of research.
Funds can be used to cover:
- Material and consumable costs.
- Equipment costs will be considered on a case-by-case basis as the SOW has been designed to not require the use of specialist technology. Please contact the T1DGC Research Funding Team to discuss this further.
- Project manager/co-ordinator costs are strongly encouraged but need to be fully justified within the application.
- Staff salaries. For example: technicians, research assistants, postdoctoral researchers*. Applicants are encouraged to include named staff on proposals.
- Travel and accommodation costs to visit collaborating institutes.
*Allowed/disallowed salary costs
- Studentships are an ineligible cost for this funding call.
- Diabetes UK will also not pay salaries on a cost recovery basis or for those already in receipt of a salary equivalent to 1FTE and is, therefore, unwilling to meet the salary costs of staff currently fully funded by the Higher Education Funding Council, NHS or equivalent. This usually applies to all Principal Applicants, Co-Applicants and Collaborators.
- Where staff salaries are dependent on grant funding, we would require a letter from the Host Institute confirming they will not be in receipt of more than 1FTE for the duration of the award, if successful.
- Diabetes UK will pay for named staff with specific expertise.
- Costs for National Insurance contributions and any superannuation should be added to salary costs at the point of application. These costs will not be considered after an award has been made. Known salary increments may be included on the application form but national pay awards may not.
- If you are unsure if the salary of a post will be covered, please contact the office to clarify.
To apply
You can submit your application via the online grant’s portal. We also encourage you to reach out to the T1DGC Research Funding Team to discuss the opportunity further before you apply.
About the Advanced Regenerative Manufacturing Institute (ARMI)
The Advanced Regenerative Manufacturing Institute (ARMI), headquartered in Manchester, New Hampshire, is a not-for-profit, Member-driven, public-private partnership found to bring the scalable, consistent, cost-effective manufacture of life-saving, cell-based technologies to scale. Bolstered by the expertise of nearly 200 industry, academic, and civic Members, ARMI is building a new industry: biofabrication, that will transform the future of healthcare and restore health and quality of life for patients, families, and communities around the globe.

The Grand Challenge community – “Work differently, work collaboratively, work swiftly”
December 4, 2024
In November, we hosted our Beta Cell Therapy and Root Causes Symposium, uniting the rapidly growing Type 1 Diabetes Grand Challenge community. More than 100 researchers, people with lived experience of type 1 diabetes, and collaborators came together for the first time. It was a space to share progress and fresh ideas, and to explore new collaborative opportunities, leveraging the diverse expertise within the community. Importantly, we also got to hear how people affected by type 1 diabetes have been working with research teams to ensure the discoveries and treatments scientists pursue are grounded in their needs.
Dr Mirjam Eiswirth, who lives with type 1 diabetes and leads the Patient and Public Involvement activities for Prof Shareen Forbes and Dr Lisa White’s project, was one of our speakers. Here, she shares her thoughts on the symposium.
“£50 million – that’s the incredible amount of money that the Steve Morgan Foundation has dedicated to the Type 1 Diabetes Grand Challenge towards the race for a cure. It’s a marathon, not a sprint, but as we heard at the Symposium – we’re well on track.”

Mirjam speaking at the symposium
A meeting of minds
107 experts from 27 institutes across 8 countries and nations gathered in London for the first time to focus on two of the Grand Challenge’s strands:
- Root causes of type 1 diabetes: what is it that makes the immune system attack the pancreas, and how can we stop this?
- Replacing beta cells: once the beta cells have been destroyed, how can we replace them with new, functioning ones to give the body a chance to make insulin again?
Can we restore insulin production in the body?
We heard about innovative approaches Grand Challenge researchers are exploring to make beta cell transplants better, more efficient, and have fewer side effects. Or to even help existing healthy pancreatic cells morph into beta cells, so that the body can produce its own insulin again. Because, as Sarah Gatward, one of the experts by experience, so neatly put it: “Nothing can control blood glucose better than beta cells.”
Could we stop type 1 diabetes from developing?
The second key theme was understanding what happens in the body that makes it turn against itself and destroy beta cells in type 1 diabetes. If we could stop this immune attack early and protect the beta cells, we could potentially stop type 1 diabetes from developing at all.
Grand Challenge teams told us about the innovative ways they’re hoping to do this, and some of the challenges to tackle along the way. We’d need to catch people early on the path to type 1 diabetes, which means we need good ways to screen for it. And we’d need to make sure we only stop the specific immune reaction at the root of type 1 diabetes, rather than suppressing the whole immune system.
Putting people with lived experience at the centre of the Grand Challenge
The Type 1 Diabetes Grand Challenge models the collaborative and disruptive spirit it champions: By including people with the lived experience from the get-go and every step on the way.
Several experts by experience, including myself, gave updates on the different ways we’re getting involved, including reviewing research proposals, as patient and public involvement co-investigators, and as sounding boards when it comes to the applicability of any novel therapy the scientists develop. Because we can ask those uncomfortable “so what” questions or say, “this therapy only makes sense to me if it helps me for more than a year or two – it needs to be a proper cure”.
For the researchers in the room, hearing more about our involvement, perspectives, and why they matter was invaluable. Dr Craig Beall, lead researcher, said: “Hearing the voices of experts by experience was inspirational and at times emotional.”
Anonymous feedback also reflected this:
Expert by experience: “I felt I was able to help inform researchers and others of what their research means to those living with type 1 diabetes and I feel confident that my input has been taken on board and will be used to influence what they do and how they present their research. ”
Early-career researcher: “I met several experts by experience and it really hammered home the importance of our research. I was astounded by the incredible role experts by experience played in shaping grant applications and steering research objectives.”

Experts by experience talking about involving people living with type 1 diabetes at the symposium
Many perspectives, lively debates
Senior researchers, early career researchers, and not least people with lived experience of type 1 diabetes shared their thoughts, hopes and projects related to the Grand Challenge. What unites us all is the vision of creating a world where diabetes can do no harm – and to be creative, think out of the box, work collaboratively, and work swiftly.
One researcher summed it up: “It felt like a community, which was great.”

Delegates chatting at the symposium
Looking ahead
Personally, I am very excited about the progress we’ll make through these research projects. They have the potential to change the lives of millions of people with type 1 diabetes for the better. A cure is still years, if not decades away – the journey to breakthroughs is a long and complex one. We need to move from discoveries in the lab, to testing new treatments with people in clinical trials, to ensuring widespread access to cures. But it’s a path filled with incredible moments of innovation and hope. And I find myself just as excited for the journey as the destination.
Researchers, practitioners and experts by experience working closely together, driven by shared ambition, can really make a difference.
You may also be interested in
Insulin on the brain
Dr Craig Beall and Dr Thomas Piers’ Beta Cell Therapy Innovation Project Grant

Led by Drs Craig Beall and Thomas Piers at the University of Exeter, this project will explore whether a type of cell found in the brain can help beta cells to make more insulin while hiding them from the immune system’s attack. Using ‘organ-on-a-chip’ devices, their approach could improve the outcomes of beta cell transplants.
Background to the research project – brain cells for beta cells
In type 1 diabetes, the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. But beta cells aren’t the only cells that make insulin, and the pancreas isn’t the only place in the body where insulin is made.
Insulin is produced in the brain. There are at least six different types of brain cells that make insulin, and in type 1 diabetes these are hidden from the immune system attack. The cells all have different functions but the insulin they produce isn’t released in the right place or in high enough quantities to help manage blood sugar levels in type 1 diabetes.
Dr Craig Beall and Dr Thomas Piers are investigating if a type of brain cell can be engineered to work together with beta cells to make lots of insulin, out of sight from the immune system. The hope is that this could help improve the effectiveness of beta cell transplants in people with type 1 diabetes.
What will the team do in this project?
In the lab, Dr Beall and Dr Piers will grow clusters of insulin-producing brain cells and beta cells on a special plate called an ‘organ-on-a-chip’ device. They’ll recreate the conditions of type 1 diabetes, and test how these clusters react to sugar, nutrients, and treatments, compared to clusters of beta cells from human donors.
They’ll also test how well blood vessels form around them on the organ-on-a-chip device as this will be important for keeping the cells alive when transplanted.
How will this research help people with type 1 diabetes?
In current beta cell transplants, the immune system tends to attack transplanted beta cells, meaning some of the benefits of transplants are short-lived. Or people who’ve had transplants need to take drugs that dial down their immune system, called immunosuppressants. Dr Beall and Dr Piers’ project could lead to the development of new or improved beta cell therapies that can help people with type 1 produce insulin for longer periods without the need for immunosuppressant drugs.
Dr Craig Beall said:
“We are really excited to have this funding from the Type 1 Diabetes Grand Challenge. This scheme really pushed us to harness brainpower to come up with the best possible ideas and to look for creative new concepts. The moonshot we’re aiming for is a cure that frees people with type 1 diabetes from insulin injections and immunosuppression, and this is the next step in that journey.“
Q&A with Professor Simon Heller
We spoke to Professor Simon Heller, world-renowned diabetes specialist and Chair of the Type 1 Diabetes Grand Challenge Scientific Advisory Panels, to find out about his research journey and hopes for the Grand Challenge
February 10, 2023
Professor Simon Heller is chair of all three scientific advisory panels in the Type 1 Diabetes Grand Challenge, covering beta cells, novel insulins and root causes of type 1 diabetes. Along with the leading experts who sit on these panels, Simon will help to steer the direction of the Grand Challenge to make sure our funding is invested in the right places, with the biggest potential to change the lives of people with type 1 diabetes. He is also Professor of Clinical Diabetes at the University of Sheffield and a world-renowned scientist, whose research has led the way in transforming our understanding of hypoglycaemia.
Why did you want to get involved with the Type 1 Diabetes Grand Challenge?
Simon: “It was a huge honour to be asked to assist in determining how this huge amount of funding could best be used to benefit type 1 diabetes research in the UK. It’s important to me to do my best to see our research move more quickly towards a cure for people with type 1.”
How do you think the Type 1 Diabetes Grand Challenge will be a game-changer for type 1 diabetes research?
“I hope that the Type 1 Diabetes Grand Challenge will allow the UK to play a major part in moving the research landscape closer to a cure. It will hopefully enable us to do something much more rapidly than we otherwise would be able to.”
What would a cure for type 1 diabetes look like to you?
“A cure would be removing the burden of day-to-day self-management of type 1 diabetes. In particular, it would allow people with the condition to live a life of spontaneity and doing activities which those of us without diabetes often take for granted.”
How did you get into the field of type 1 diabetes research?
“When I arrived at the Queens Medical Centre in Nottingham as a trainee registrar, I was intending to be a cardiologist. But a six-month placement in a diabetes team changed that. The legendary diabetes researcher Robert Tattersall (who discovered MODY and introduced the world to self-monitoring blood glucose levels) was my boss. He was a wonderful teacher who taught me to listen to people with diabetes and learn for myself how much it asked of people in terms of self-management. He also showed me that it wasn’t the healthcare professionals who made the biggest impact on managing type 1, but instead how much the person themselves could learn and implement about this very complex condition. Robert inspired me to become a researcher and showed me what an interesting and important specialty diabetes is.”
What has been your career highlight so far?
“It’s hard to narrow it down. One highlight is bringing the DAFNE training course – which helps people with type 1 lead a healthy life – from Germany to the UK’s NHS. Another key achievement was discovering that repeated hypos lead to impaired awareness of hypoglycaemia and increased risk of hypoglycaemia. I feel fortunate that I have been involved in research which has made a difference to the lives of people with type 1.”
Tell us something we don’t know about diabetes or the pancreas
“When I was preparing a talk on hypoglycaemia, I learnt that the first definition of 1 unit of insulin was the amount of insulin which could cause an epileptic seizure in a rabbit. This is because over a hundred years ago when insulin was discovered, there was no way of measuring insulin amounts. I read this fact in a wonderful book by Michael Bliss titled The Discovery of Insulin.”
What are you currently working on?
“My main research project at the moment is working with researchers from the USA, UK and Australia on a large research trial. The study is testing what the most effective way of restoring the warnings for hypoglycaemia in people with type 1 who have lost them.”
What skills do you need to have to be a great researcher?
“From working with great researchers, I’ve learnt that they need to be curious, creative and persistent. The best clinical researchers listen to people with lived experience to ensure they address important questions.”
What do you like doing when you’re not working on research?
“I spend my spare time travelling to interesting places, reading, and listening to music – particularly opera. I also love spending time with my family and my three grandkids. Less rewarding in recent years has been my love for Tottenham Hotspur FC.”
What would you be doing if you weren’t a researcher?
“I can’t think of any other careers as rewarding as supporting patients. I’d be very happy just doing clinical work alone.”
Q&A with Professor Simon Heller
We spoke to Professor Simon Heller, world-renowned diabetes specialist and Chair of the Type 1 Diabetes Grand Challenge Scientific Advisory Panels, to find out about his research journey and hopes for the Grand Challenge
November 22, 2022
Professor Simon Heller is chair of all three scientific advisory panels in the Type 1 Diabetes Grand Challenge, covering beta cells, novel insulins and root causes of type 1 diabetes. Along with the leading experts who sit on these panels, Simon will help to steer the direction of the Grand Challenge to make sure our funding is invested in the right places, with the biggest potential to change the lives of people with type 1 diabetes. He is also Professor of Clinical Diabetes at the University of Sheffield and a world-renowned scientist, whose research has led the way in transforming our understanding of hypoglycaemia.
Why did you want to get involved with the Type 1 Diabetes Grand Challenge?
Simon: “It was a huge honour to be asked to assist in determining how this huge amount of funding could best be used to benefit type 1 diabetes research in the UK. It’s important to me to do my best to see our research move more quickly towards a cure for people with type 1.”
How do you think the Type 1 Diabetes Grand Challenge will be a game-changer for type 1 diabetes research?
“I hope that the Type 1 Diabetes Grand Challenge will allow the UK to play a major part in moving the research landscape closer to a cure. It will hopefully enable us to do something much more rapidly than we otherwise would be able to.”
What would a cure for type 1 diabetes look like to you?
“A cure would be removing the burden of day-to-day self-management of type 1 diabetes. In particular, it would allow people with the condition to live a life of spontaneity and doing activities which those of us without diabetes often take for granted.”
How did you get into the field of type 1 diabetes research?
“When I arrived at the Queens Medical Centre in Nottingham as a trainee registrar, I was intending to be a cardiologist. But a six-month placement in a diabetes team changed that. The legendary diabetes researcher Robert Tattersall (who discovered MODY and introduced the world to self-monitoring blood glucose levels) was my boss. He was a wonderful teacher who taught me to listen to people with diabetes and learn for myself how much it asked of people in terms of self-management. He also showed me that it wasn’t the healthcare professionals who made the biggest impact on managing type 1, but instead how much the person themselves could learn and implement about this very complex condition. Robert inspired me to become a researcher and showed me what an interesting and important specialty diabetes is.”
What has been your career highlight so far?
“It’s hard to narrow it down. One highlight is bringing the DAFNE training course – which helps people with type 1 lead a healthy life – from Germany to the UK’s NHS. Another key achievement was discovering that repeated hypos lead to impaired awareness of hypoglycaemia and increased risk of hypoglycaemia. I feel fortunate that I have been involved in research which has made a difference to the lives of people with type 1.”
Tell us something we don’t know about diabetes or the pancreas
“When I was preparing a talk on hypoglycaemia, I learnt that the first definition of 1 unit of insulin was the amount of insulin which could cause an epileptic seizure in a rabbit. This is because over a hundred years ago when insulin was discovered, there was no way of measuring insulin amounts. I read this fact in a wonderful book by Michael Bliss titled The Discovery of Insulin.”
What are you currently working on?
“My main research project at the moment is working with researchers from the USA, UK and Australia on a large research trial. The study is testing what the most effective way of restoring the warnings for hypoglycaemia in people with type 1 who have lost them.”
What skills do you need to have to be a great researcher?
“From working with great researchers, I’ve learnt that they need to be curious, creative and persistent. The best clinical researchers listen to people with lived experience to ensure they address important questions.”
What do you like doing when you’re not working on research?
“I spend my spare time travelling to interesting places, reading, and listening to music – particularly opera. I also love spending time with my family and my three grandkids. Less rewarding in recent years has been my love for Tottenham Hotspur FC.”
What would you be doing if you weren’t a researcher?
“I can’t think of any other careers as rewarding as supporting patients. I’d be very happy just doing clinical work alone.”