At the Type 1 Diabetes Grand Challenge, we support cutting-edge research aimed at bringing us closer to better treatments, and potentially, a cure. The research teams we fund are leaders in the field and their latest discoveries, highlighted here, are contributing to global efforts to transform the treatment of type 1 diabetes.
Connection between a common virus and type 1 diabetes
The development of type 1 diabetes is caused by a complex interplay of genetic and environmental factors, which trigger the immune system to turn on and destroy insulin-producing beta cells. The Type 1 Diabetes Grand Challenge is investing in research to learn more about precisely what goes wrong and how this process unfolds.
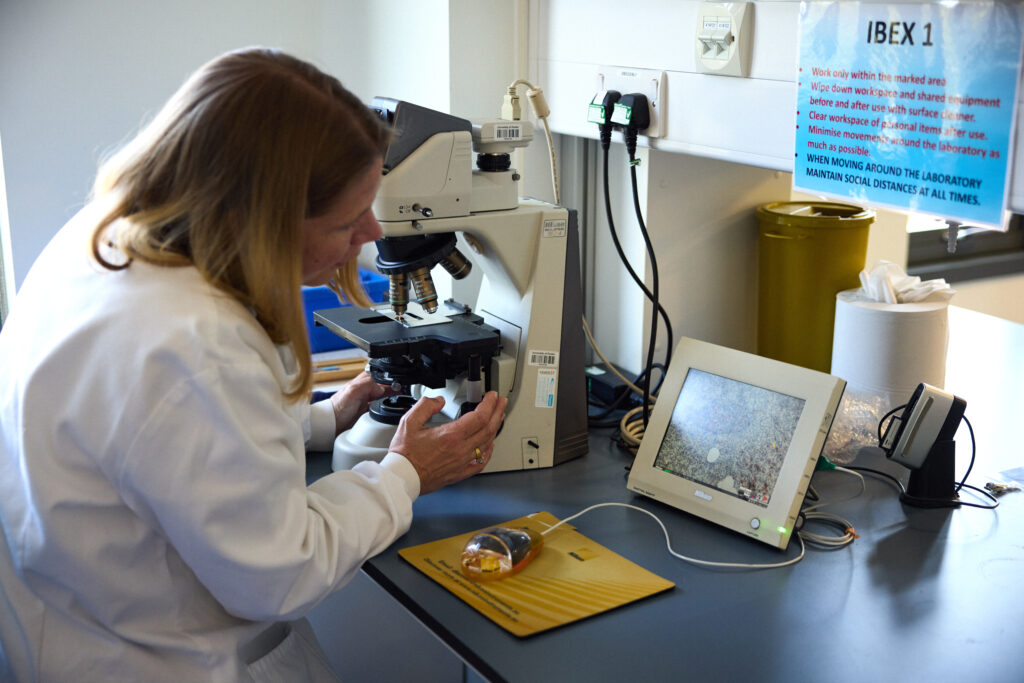
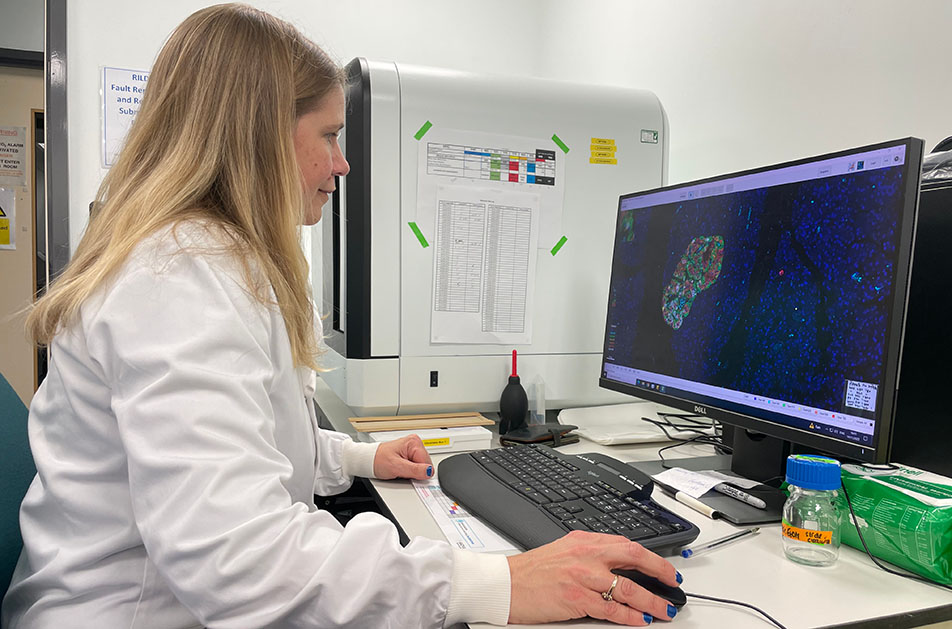
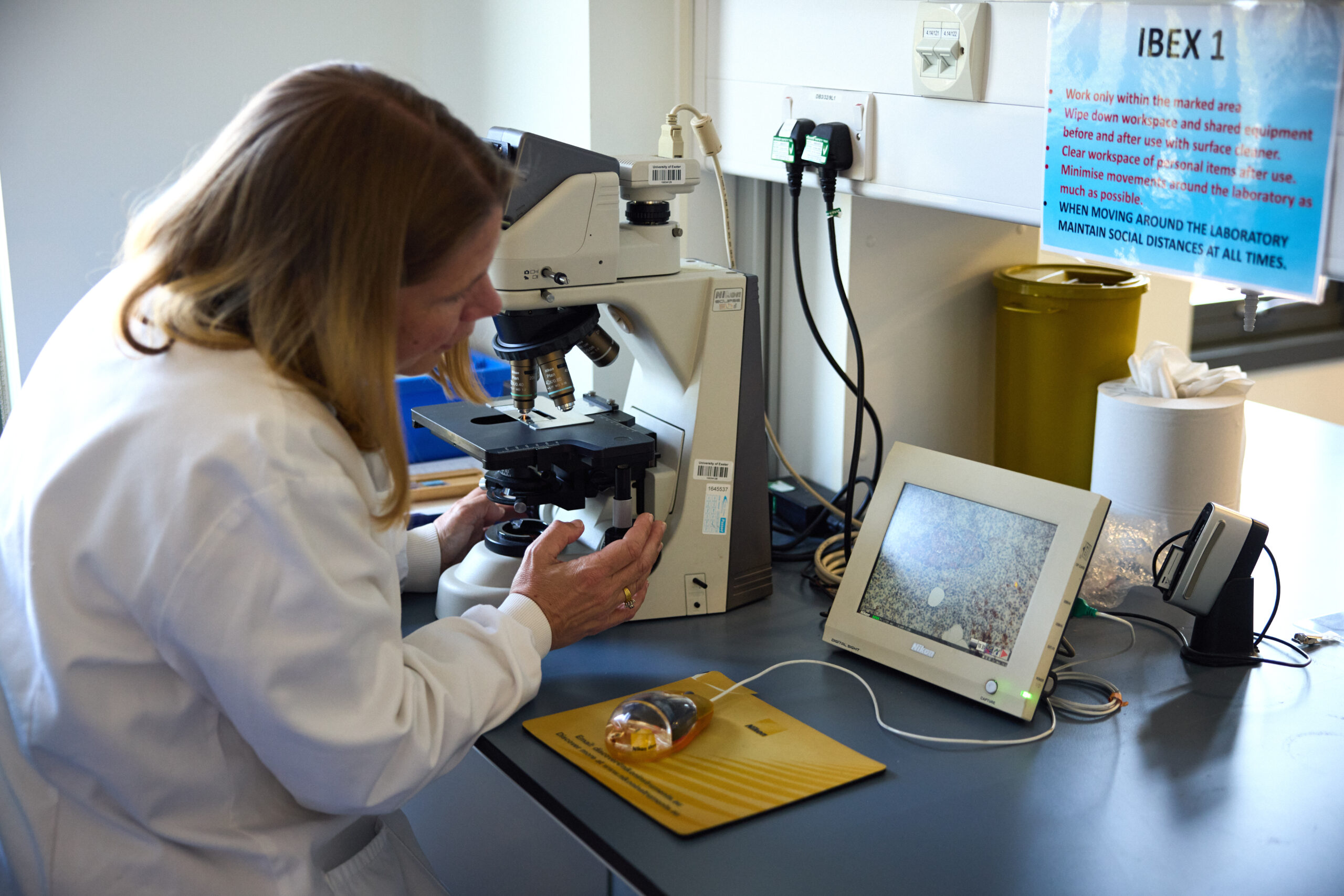
An international research team, including our Senior Research Fellow Professor Sarah Richardson, has just published the strongest evidence to date that enteroviruses play a role in the development of type 1 diabetes.
They studied pancreas samples from nearly 200 donors to check for signs of enterovirus infections. These included samples from people with and without type 1 diabetes, as well as individuals who had type 1 diabetes autoantibodies – early immune warning signals that indicate a high risk of developing the condition in the future.
They reported that signs of enterovirus infection were most common in people with type 1 diabetes who still had some functioning beta cells. Infections were also present in people with autoantibodies, but much less common in those without diabetes or in people with type 1 whose beta cells had already been completely destroyed.
A key finding was the presence of a protein made by the enterovirus, called VP1. The researchers found VP1 was strongly linked to high levels of HLA class I molecules. These are markers of an early immune system response in the pancreas. This is the first time these viral and immune markers have been found together – including in the early stages of type 1 before a diagnosis.
These findings offer the strongest evidence to date that enteroviruses may trigger or accelerate the onset of beta cell destruction in early type 1 diabetes. A clearer understanding of their role could lead to new approaches that target the immune processes they influence — potentially slowing or even preventing type 1.
‘Ticking’ beta cell protection
One part of a solution to curing type 1 diabetes is to transplant beta cells, either donated or grown in labs, into people with type 1 so they could produce their own insulin again. However, the immune system is primed to attack the new cells too. This happens partly because the transplanted cells release chemokines—chemical signals that attract immune cells. Blocking these signals is difficult, as there are many different types.
Scientists have discovered that ticks produce proteins called evasins that can block several of these signals at once. Professor Shoumo Bhattacharya’s team has studied these evasin proteins and identified the specific peptides that have this powerful blocking ability. They’ve established a new method that allows them to test many versions of these peptides rapidly, and pinpointed those that work best at calming the immune response.
Published in Communications Biology, these innovative findings lay the groundwork for Professors Shoumo Bhattacharya and David Hodson’s Grand Challenge project. They aim to use these peptides to help protect new beta cells from immune attack after being transplanted. This could create a safer alternative to immunosuppressive drugs and improve the success of beta cell therapies for type 1 diabetes.
Giving insulin a smart coat
Professor Zhen Gu’s team at Zhejiang University in China has developed a new insulin delivery system, called i-crystal, as reported in their latest publication in Nature Nanotechnology.
Designed to help people with type 1 diabetes keep blood sugar levels within target range, the system uses specially coated insulin crystals that release insulin slowly and steadily. The coating is a unique membrane that enables the crystals to respond precisely to changes in blood sugar and ketone levels. This means insulin is only released when blood sugar levels rise and stops when it drops, helping people with type 1 avoid highs (hypers) and lows (hypos).
Early tests show that i-crystal could help regulate blood sugar levels for over a month in mice after just one injection, and for more than three weeks in minipigs after five daily doses. This suggests this delivery system could reduce the need for frequent injections and make daily diabetes management easier.
If successful, i-crystal could offer a safer, longer-lasting, and more adaptable form of insulin therapy for people living with type 1 diabetes.
The Type 1 Diabetes Grand Challenge makes waves at DUKPC
The Type 1 Diabetes Grand Challenge took centre stage at this year’s Diabetes UK Professional Conference, uniting researchers and people affected by type 1 diabetes to share their expertise and celebrate progress with the wider diabetes community.
March 14, 2025
The Type 1 Diabetes Grand Challenge took centre stage at this year’s Diabetes UK Professional Conference, uniting researchers and people affected by type 1 diabetes to share their expertise and celebrate progress with the wider diabetes community.
Our community in the spotlight
The main Grand Challenge session was a powerful showcase of our ever-growing community, featuring 13 new projects we’ve funded in the last year.
The session began with updates from researchers working to build better beta cells in the lab from stem cells, protect new cells during and after transplantation, and regrow beta cells in people with type 1 diabetes.
Later on in the conference, we heard more about islet transplantation, using cells from donor pancreases. Prof Shareen Forbes discussed the potential of microparticle drug delivery to protect transplanted islets and improve their survival. And we were joined by Dr Vicky Salem who highlighted innovations in biomaterials that could transform islet transplantation.
Our immune insights project leads shared exciting progress on targeting the type 1 immune system attack in safer and more effective ways. Dr James Pearson revealed that some immune cells follow a daily rhythm, and that’s why his project is testing if immunotherapies timed to these cycles will improve their effectiveness.
We also welcomed Profs Michael Weiss, Matthew Webber and Zhiqiang Cao, who discussed their eye-opening ideas to develop novel insulins that could act more quickly and precisely, ultimately reducing the burden of type 1 diabetes management.

Picture of Profs Michael Weiss, Matthew Webber accepting their awards; credit: © Julie Broadfoot
You can find more details about each project presented at DUKPC on our funded projects page.
Lived experience at the heart of research
A dedicated session at DUKPC highlighted how the quality and impact of Grand Challenge research is being enhanced by meaningfully involving people with lived experience of type 1.
Heather Robinson, a Together Type 1 young leader, shared striking statistics on the difficulties of transitioning from paediatric to adult diabetes care, underscoring the need for greater involvement from those directly affected.
Dr James Pearson echoed this, sharing how the challenge of recruiting young adults with type 1 for research led him to involve them more actively through the Cardiff Diabetes Innovation Committee. Committee members reflected on how this engagement deepened their understanding of type 1 diabetes and ensured research truly benefits those who need it most.

Picture of Dr James Pearson and Lilly from the Cardiff Diabetes Innovation Committe; credit: © Philippa Gedge Photography
Recognising the importance of lived experience in research, Professor Sean Dinneen spoke about working with young adults with type 1 to identify gaps in care and improve treatments, while Dr O’Donnell showcased his project co-developing user-led technology that prioritises real-life experiences and emotional well-being.
Amelia Burke, a glass artist from Wales and mum of Ruby who lives with type 1, emphasised that involvement must be accessible and approachable. Her interactions with Grand Challenge researchers inspired her to use artistic methods to represent her daughter’s experience and raise awareness about beta cell therapies.
Heather shared her experience at the conference with us:
“Getting to experience DUKPC from multiple perspectives was such a unique and unforgettable opportunity. From interviewing researchers, speaking on a panel, meeting other Young Leaders from the Together Type 1 program and presenting in the Grand Challenge Patient and Public Involvement session, it was a jam-packed few days! Being able to watch the involvement of experts by experience increase over the past few years has been brilliant, and with the collaboration of Steve Morgan Foundation, Diabetes UK and Breakthrough T1D has only developed this. Speaking with researchers and experts by experience brought such a broad range of viewpoints and I’m so excited for the future of patient-led diabetes research and healthcare.”

Picture of Heather with Dr Craig Beall at DUKPC
Bringing research to reality
For research to truly make an impact, scientific breakthroughs must be translated into real-world solutions. And that’s exactly what we’re aiming to achieve through the Grand Challenge— accelerating great ideas to change the lives of those affected by type 1 diabetes. As part of this, we hosted a ‘Top Tips on Commercialisation’ session, bringing together experts in research funding, policy, and entrepreneurship to share practical advice on turning research into real-world impact. This is just the beginning —throughout this year we’ll continue to support our community in in moving innovations from the lab into people’s lives.
Dr Andy Chapman, CEO and Co-Founder of Carbometrics says:
“Thank you to Type 1 Diabetes Grand Challenge for inviting me to speak at the Diabetes UK Professional Conference 2025 in Glasgow. It was a privilege to join such an esteemed panel to discuss the challenges and future of commercialisation in diabetes technology, and connect with fellow innovators in this space.”
Dr Bethany Cragoe, Charity Business Manager of LifeArc, says:
“Charities are crucial in getting research to patients by leveraging the expertise of many stakeholders including patients, scientists, clinicians, and industry partners. Technology transfer is key in this process, and early engagement with technology transfer offices helps develop effective intellectual property strategies and potential routes to patient benefit.
“Researchers should understand the translational pathway and plan early to ensure their work benefits patients. Building strong networks with industry and funders is key to success in this journey. Organisations and initiatives such as Knowledge Exchange UK, Innovate UK and Association of Technology Transfer Professionals can support this. All these elements must come together to ensure that the funded research outputs are able to realise their maximum potential for patient benefit.”

Picture of Dr Bethany Cragoe speaking at the ‘Top Tips on Commercialisation’ credit: © Philippa Gedge Photography
New funding available to boost beta cell research in the UK
December 20, 2024
We’re launching a new funding call to address the limited availability of stem cell-derived beta cells for research purposes.
The aim is to facilitate more high-quality research into beta cell therapies, speeding up progress towards a cure for type 1 diabetes.
To achieve this, we’ve partnered with the Advanced Regenerative Manufacturing Institute (ARMI), the US leading organisation in manufacturing cells, tissues and organs.
Funding is available for UK-based researchers to test if stem cell-derived beta cells produced by ARMI can survive shipment from the US to the UK. And if they can, whether they work as expected in both lab studies and living organisms.
We’re inviting UK experts with a track record of producing and testing stem cell-derived beta cells to apply for funding to test ARMI’s beta cells. Funding is available for up to three sites across the UK.
Successful researchers will also have the opportunity to directly compare ARMI’s beta cells with their own lab-made beta cells. This may help them to improve their own production process and identify the most effective product for wider rollout.
The hope is that it will enable the development of a reliable supply of high-quality, pre-made stem cell-derived beta cells for use by UK scientists. By saving researchers time and ensuring consistency across studies, this initiative is expected to accelerate the development of new beta cell replacement therapies.
Apply for funding
Details about the call can be found here. You’ll need to submit your application by 31 January 2025.
If you’re interested in applying, we strongly encourage you to attend our funding call webinar on 8 January 2025 at 14:00 GMT and reach out to the T1DGC Research Funding Team to discuss the opportunity further (smfgrandchallenge@diabetes.org.uk).
The Advanced Regenerative Manufacturing Institute (ARMI | BioFabUSA) said:
“ARMI is proud to partner with the Type 1 Diabetes Grand Challenge to advance beta cell research. By providing high-quality, stem cell-derived beta cells for validation, we aim to accelerate breakthroughs in type 1 diabetes treatment and improve the scalability of regenerative therapies. This initiative represents a critical step in bridging global efforts to bring innovative solutions to patients.”
Professor Matthias Hebrok, Vice Chair of the Type 1 Diabetes Grand Challenge Scientific Advisory Panel, said:
“Testing stem cell derived islets produced by a foundry for their functional properties upon being sent to the UK is critical to ensure high quality tissues will be available to accelerate research in type 1 diabetes.”
Gaining pace towards a cure – a round-up of 2024
December 16, 2024
The global quest to create better treatments and find ways to prevent and cure type 1 diabetes continued to gather pace in 2024. At the Type 1 Diabetes Grand Challenge, we kickstarted 10 pioneering research studies across the UK and globally, expanding our portfolio of funded science to 19 projects, involving 161 researchers in 47 institutions across 8 countries, and shared our mission with thousands affected by the condition.
Here, we round-up the highlights of the year.
Science fiction into fact
The Type 1 Diabetes Grand Challenge is taking the quest to cure type 1 diabetes to a new level by emboldening scientists to be innovative and disruptive, leading to totally new avenues of discovery. That’s why some of the projects funded in 2024 read like sci-fi storylines, from investigating insulin-producing brain cells to copying the immune evasion tactics used by ticks.
This year, we invested over £2 million into four new research projects to tackle the root causes of type 1 and replace the insulin-making beta cells lost in type 1. Four research teams are now hard at work on these innovative ideas, and others.
Dr Elizabeth Robertson, Director of Research at Diabetes UK, said: “These high-risk, high-reward, innovative projects exemplify the transformative potential of the research funded by the Type 1 Diabetes Grand Challenge. By driving forward bold, cutting-edge approaches, we’re stepping closer to revolutionising the way type 1 diabetes is treated and improving the lives of those affected by the condition.”
One of the newly funded researchers, Dr Craig Beall, summed up the ambition: “The moonshot we’re aiming for is a cure that frees people with type 1 diabetes from insulin injections and immunosuppression.”
Innovating insulin
For over a century, type 1 diabetes has been treated with insulin. It’s a life-saving treatment, but it’s also a very blunt instrument, unable adapt to the wide-ranging factors that affect blood glucose levels.
In August 2024, we invested over £2.7 million into six projects to develop ‘smart’ insulins that could transform the treatment of type 1. The six research teams are aiming to create next-generation insulins that can respond to changing blood glucose levels, ultrafast-acting insulins and a combination drug that can both raise and reduce glucose levels.
Rachel Connor, Director of Research Partnerships at Breakthrough T1D, said: “Managing glucose levels with insulin is really tough, and it’s time for science to find ways to lift that burden. By imagining a world where insulins can respond to changing glucose levels in real-time, we hope these six projects will help to create that new reality, relieving people with type 1 of the relentless demands that living with this condition places on them today.”
On tour with the Grand Challenge
People affected by type 1 diabetes are at the heart of the Grand Challenge. It was born out of Steve and Sally Morgan’s family experience of type 1, and we actively involve those living with type 1 diabetes at every stage of the research process — from shaping funding decisions to playing a crucial role in supporting researchers in delivering their projects.
So, in 2024, we took the Grand Challenge into the community, talking to thousands of people who understand the day-to-day struggle of type 1 and the importance of our mission to revolutionise treatments and find cures.
We were delighted to join DiabetesChat’s fifth virtual research event, and to attend the Talking About Diabetes (TAD) event in Liverpool. At TAD 2024, Liam Eaglestone, CEO of the Steve Morgan Foundation, and his son Jack, took to the stage to talk about their experiences of living with type 1. Liam said: “[Diabetes] Technology is great – but it is not a cure. The Grand Challenge is seeking that cure, by bringing together some of the best and brightest brains in the type 1 research community.”
We were joined at the Diabetes UK Professional Conference by seven Young Leaders from the Together Type 1 programme. These inspiring young advocates interviewed Grand Challenge researchers and shared their experiences of living with type 1 with scientists and healthcare professionals. And in November, some of the Grand Challenge team visited Northern Ireland to give the Together Type 1 Young Leaders there an update on the latest research developments.
Young Leader Elisa Featherstone said: “Hearing about this research programme made me consider, for the first time, the reality of not having type 1 diabetes for the rest of my life. A cure may be sooner than we think, and it may well be because of the Grand Challenge!”
Progress through collaboration
Collaboration is key to progress, a principle exemplified at our first Beta Cell and Root Causes symposium held in November 2024. The symposium brought together hundreds of researchers from different strands of the Grand Challenge and people living with type 1 diabetes.
Dr Mirjam Eiswirth, who lives with type 1 diabetes and wrote a summary of the symposium, said: “Personally, I am very excited about the progress we’ll make through these research projects. They have the potential to change the lives of millions of people with type 1 diabetes for the better.”
Simon Heller, Chair of the Scientific Advisory Panel, said: “We’re moving faster than I thought we would. The willingness of scientists to collaborate shows what can be achieved when we work together.”
At the symposium, the first recipients of Grand Challenge funding, our Senior Research Fellows Professor Sarah Richardson, Dr James Cantley and Dr Victoria Salem, highlighted the remarkable progress their projects have made over the past year. Early career researchers in Dr Cantley’s lab have taken pancreatic cells from mice and regrown them into beta cells – they will now search for drugs that can support this process. Professor Richardson’s team has found that small clusters of beta cells, common in young children, are more vulnerable to the autoimmune attack. Lastly, researchers in Dr Salem’s team is engineering a device that can protect lab-grown beta cells from the immune attack while providing nutrients via a blood supply. We’re excited to track the the trio’s progress in 2025!
Looking ahead with hope
The Type 1 Diabetes Grand Challenge will continue to build momentum in 2025. We’ll begin to see early outcomes from our first projects and will invest in more disruptive and collaborative science.
Building on the conversations sparked at the symposium, we look forward to the Grand Challenge advancing through collaborative working, and we’re excited to continue this progress at the Diabetes UK Professional Conference in February, where Grand Challenge researchers will share ideas and forge new connections.
As Sally and Steve Morgan said: “It’s about doing things differently, it’s about taking risks, but above all it’s about collaboration. Let’s work as a team.”
Four innovative projects receive funding from the Type 1 Diabetes Grand Challenge
October 22, 2024
We’re investing over £2 million into four new research projects exploring creative approaches to improve beta cell therapies and tackle immune system dysfunction in type 1 diabetes.
The latest batch of cutting-edge projects are now underway thanks to funding from the Grand Challenge. This investment will help research teams across the UK to test their original and potentially groundbreaking ideas on ways to improve the function and survival of insulin-producing beta cells and keep the type 1 immune attack at bay. Together, these pioneering projects offer new hope to improve the lives of people with type 1 diabetes.
Tiny molecules with big potential
Dr Aida Martinez-Sanchez, Dr Prashant Srivastava and their team at Imperial College London, along with Dr Teresa Rodriguez-Calvo at Helmholtz Zentrum Munich, will study how microRNAs – tiny molecules in our cells that switch different genes on and off and change how the cell works – affect the function and survival of beta cells.
Dr Aida Martinez-Sanchez said:
“The complex methodologies we’re developing have the potential to form the basis of future research in other important aspects of beta cell biology, such as how to reduce the risk of transplant rejection, or delay or prevent beta cell destruction in type 1 diabetes.”
Read more about the team’s project.
Insulin on the brain to outsmart type 1
At the University of Exeter, a team led by Dr Craig Beall and Dr Thomas Piers will explore whether a type of brain cell that produces insulin can be used to develop long-lasting, effective beta cell therapies for type 1 diabetes which are resistant to the type 1 immune attack.
Dr Craig Beall said:
“The moonshot we’re aiming for is a cure that frees people with type 1 diabetes from insulin injections and immunosuppression, and this is the next step in that journey.”
Read more about the team’s project.
Developing drugs from bugs – how do beta cells tick?
Tick saliva contains peptides that helps to hide them from their victims’ immune systems. Researchers at the University of Oxford led by Professor Shoumo Bhattacharya and Professor David Hodson will harness these immune system evading peptides to develop beta cell therapies that are protected from the type 1 immune attack. This could transform the way the condition is treated by helping people to make their own insulin again without the need for immunosuppressive drugs.
Professor Shoumo Bhattacharya said:
“Our lab is looking to nature for new ways to treat inflammatory diseases. We aim to develop tick-inspired treatments to help people with type 1 diabetes, which could improve the success of beta cell transplants.”
Read more about the team’s project.
Could an existing medicine reverse the steps that lead to type 1 diabetes?
Professor Eoin McKinney and his team at the University of Cambridge will use genetic insights and powerful machine learning technology to identify and test new drug candidates for type 1 diabetes. The team has created detailed maps of immune cell changes in people at high risk of type 1, identifying specific genetic patterns, called signatures, that are only seen in those who develop the condition. Using these signatures, they now aim to understand the abnormal immune signals that lead to type 1 diabetes and find drugs to counter them, with the aim of preventing the condition from progressing.
Professor Eoin McKinney said:
“By selecting candidate treatments rationally based on a match with type 1 data, we will stand the best possible chance of finding a safe and effective approach to stop the condition with real impact for patients everywhere.”
Read more about the team’s project.
Dr Elizabeth Robertson, Director of Research at Diabetes UK, said:
“These high-risk, high-reward, innovative projects exemplify the transformative potential of the research funded by the Type 1 Diabetes Grand Challenge. By driving forward bold, cutting-edge approaches, we’re stepping closer to revolutionising the way type 1 diabetes is treated and improving the lives of those affected by the condition.”
Rachel Connor, Director of Research Partnerships at Breakthrough T1D UK, said:
“With these new projects the Type 1 Diabetes Grand Challenges is now funding a total of 19 innovative research studies, all driving us closer to transforming life for people type 1 diabetes. Each project takes a unique approach to the three challenges in type 1 diabetes that we’re tackling: replacing beta cells, uncovering the root causes of type 1, and developing the next generation of insulins.”
New ‘smart insulin’ marks promising step forward in type 1 diabetes treatment
October 17, 2024
A new study, published in Nature, has demonstrated that in animal models, a newly developed form of insulin can switch on and off in response to changing blood glucose levels, effectively lowering high glucose levels without causing dangerous hypos.
The new insulin, named NNC2215 was developed by an international team involving companies based in Denmark, the UK, and the Czech Republic as well as the University of Bristol. It features a sophisticated molecular ‘switch’ mechanism made of two parts: a ring-shaped structure and a molecule with a similar shape to glucose called a glucoside. When blood sugar levels are low, the glucoside binds to the ring, keeping the insulin in an inactive, or ‘off’ state to prevent further lowering of blood sugar. As blood glucose rises, the glucoside is replaced by glucose itself, triggering the insulin to shift its shape and become active, helping bring blood sugar levels down to safer ranges.
‘Smart’ insulins such as this one have the potential to be truly transformative in the management of type 1 diabetes. Unlike traditional insulin, which needs to be carefully dosed to avoid hypoglycemia, a ‘smart insulin’ would only activate when needed, making it a safer and more efficient treatment.
New types of insulin like NNC2215 could lead to a significant improvement in quality of life for people living with type 1 diabetes, helping to reduce the constant burden of managing blood sugar levels.
Researchers who developed NNC2215 found it to be as effective as human insulin at lowering blood glucose in rats and pigs. No timeline has been given for the next steps in developing this product or for clinical trials in people with diabetes, but this is a significant step forward in the search for more advanced and reliable treatments for diabetes. This proof of concept highlights how clever chemistry could unlock entirely new options for people with type 1 diabetes.
Dr Tim Heise, Vice Chair of our novel insulins Scientific Advisory Panel, said:
“This elegant study shows that it is feasible to quickly switch insulin action on and off depending on prevailing glucose levels, and to minimise the risk of hypoglycaemia in pigs.
“While this study certainly is important progress, many more steps will have to follow to establish glucose-sensitive insulins as treatment for people with diabetes. Nevertheless, I am confident that the intense research in glucose-sensitive insulins including the developments funded by the Type 1 Diabetes Grand Challenge programme will manage to achieve this goal.”
Rachel Connor, Director of Research Partnerships at Breakthrough T1D in the UK, said:
“It’s exciting to see data on a new form of insulin that can change its structure to switch activity on and off as glucose levels change. This shows us that a future where people with diabetes no longer need to worry about hypos as a result of insulin therapy could be within reach.”
Dr Elizabeth Robertson, Director of Research at Diabetes UK, said:
“This research represents a significant step forward in the global effort to develop the next generation of “smart” insulins. The hope is that these will ease the constant challenge of managing blood sugar highs and lows, and improve the physical and mental health of millions of people worldwide with diabetes who rely on insulin therapy. We’re excited to part of this endeavour through our Type 1 Diabetes Grand Challenge programme.”
The Type 1 Diabetes Grand Challenge is currently funding six research projects aimed at developing new types of insulin. The goal of the research programme is to eventually offer a range of personalised treatment options for people with type 1 diabetes, tailoring therapies to meet each patient’s unique needs. This exciting progress in insulin innovation brings us one step closer to that vision.
£2.7m funding launches six new global research projects into novel insulins
August 12, 2024
We are funding six new research projects worth over £2.7 million through the novel insulins challenge to transform type 1 diabetes treatment. This vital funding will accelerate the development of insulins that more closely mimic how a healthy pancreas works, which could improve the lives of people living with type 1 diabetes.
Developing novel insulins
Today’s announcement grants over £2.7 million to six new international research projects focused on developing next-generation insulins, also known as novel insulins. This crucial research, conducted at universities in the United States, Australia, and China, aims to design insulins that act faster and more precisely, relieving some of the burden of managing type 1 diabetes and reducing the risk of long-term complications.
People with type 1 diabetes can’t make their own insulin, so they must give themselves synthetic insulin several times each day to survive. But insulin is far from a cure for type 1 diabetes, and new forms of insulin are urgently needed.
Why do we need new insulins?
Blood glucose levels are affected by many factors including food intake, exercise, stress, other hormones, and even the weather. This complexity means that even with the most advanced technology available, many people with type 1 diabetes fluctuate between high and low glucose levels, resulting in short and long-term physical health issues. The relentless struggle to stabilise blood glucose with existing insulins can also be a significant mental burden for people living with type 1 diabetes.
Glucose-responsive ‘smart’ insulins
Four of these newly funded projects involve scientists creating and testing novel insulin formulations that can respond to changing blood glucose levels, known as glucose responsive insulins (GRIs). The concept of glucose responsive insulins is that the drug only becomes active when there is a certain amount of glucose in the blood to prevent hyperglycaemia (high blood glucose) and becomes inactive again when levels drop below a certain point, avoiding hypoglycaemia (low blood glucose).
Ultrafast acting insulin
Researchers running a fifth research project are developing a new ultrafast, short-acting insulin. Even with the fastest insulins that are currently available, there is still a delay between the drug being administered and the point it starts to act on glucose in the blood. This can result in blood glucose rising to unsafe levels before insulin can act to lower it. Faster insulins are also needed to improve the function of insulin pumps and hybrid closed loop technology, a system that relies on the stored insulin responding in real-time to changing blood glucose levels.
Combining insulin and glucagon
The final research project is focused on designing a protein that combines insulin with another hormone, glucagon. Unlike insulin, which helps remove glucose from the blood, glucagon stimulates the liver to release more glucose when levels in the blood run low. Having both hormones included in one formulation could keep blood glucose levels stable by working to prevent high and low blood glucose levels.
Dr Tim Heise, Vice Chair of our Novel Insulins Scientific Advisory Panel, said:
“Even with the currently available modern insulins, people living with type 1 diabetes have to put lots of effort into managing their diabetes every day to find a good balance between acceptable glycaemic control on the one hand and avoiding hypoglycaemia on the other. The funded six new research projects address major shortcomings in insulin therapy.
Glucose-responsive (so-called ‘smart’) insulins are regarded as the holy grail of insulin as they would come as close to a cure for type 1 diabetes as any drug therapy could. A truly rapid short-acting insulin might make it finally possible to progress from hybrid to fully closed loop systems, allowing a technological ‘cure’ for insulin-treated people with diabetes. Potentially minimising the risk of hypoglycaemia through an insulin-glucagon combination would ease one of the major concerns associated with insulin therapy today. Therefore, these research projects, if successful might do no less than heralding a new era in insulin therapy.”
Professor Simon Heller, Chair of our Scientific Advisory Panel, said:
“This unique funding is transforming the ability of global scientists to join forces to tackle type 1 diabetes. It enables researchers to set up new collaborations and to test innovative ideas which may lead to a step change in finding a cure for type 1 diabetes.”
Rachel Connor, Director of Research Partnerships at JDRF UK, said:
“With this funding programme we have challenged scientists around the world to drive forward new ideas in insulin design to combat the relentless burden of managing type 1 diabetes.
While insulin has been saving lives for over a hundred years now, and previous research has driven important changes for people with type 1, it is still not good enough – managing glucose levels with insulin is really tough, and it’s time for science to find ways to lift that burden.
By imagining a world where insulins can respond to changing glucose levels in real-time, we hope these six projects will help to create that new reality, relieving people with type 1 of the relentless demands that living with this condition places on them today.”
Dr Elizabeth Robertson, Director of Research at Diabetes UK, said:
“This much needed funding boost has the potential to revolutionise type 1 diabetes treatment. By supporting these groundbreaking research projects, we are aiming to develop new insulins that more closely mimic the body’s natural responses to changing blood sugar levels. This could significantly reduce the daily challenges of managing type 1 diabetes, and improve both the physical and mental health of those living with the condition. We are hopeful that this research will lead to life-changing advancements in type 1 diabetes care.”
The Type 1 Diabetes Grand Challenge returns to DUKPC
May 7, 2024
The Type 1 Diabetes Grand Challenge was the topic on everyone’s lips at this year’s Diabetes UK Professional Conference. Many of the large and growing community of Grand Challenge researchers were in attendance to celebrate their awards and update delegates on their research plans and progress.
The drive behind the Grand Challenge
The Grand Challenge session at this year’s DUKPC was chaired by Sally Morgan, a Trustee of the Steve Morgan Foundation, who opened with an emotive speech about her family’s journey with type 1 diabetes and their hope for a cure, and Professor Simon Heller, Chair of our Scientific Advisory Panels, who introduced the speakers, our three Senior Research Fellows.
Regrowing new beta cells
First up was Dr James Cantley, who began by explaining his ambitious drug discovery work to find a drug to regenerate the beta cells that have been destroyed by the immune attack. Sometimes the process of making new beta cells (neogenesis) is restored in adults, as a result of stress or injury. Dr Cantley and his team at the University of Dundee are modelling this process in the lab, and testing the effect different drugs have on it. Their aim is to find a drug that can support beta cell regrowth and be tested in clinical trials of people with type 1 diabetes.
Dr Cantley is also exploring how to encourage existing beta cells to reproduce. The immune attack on beta cells is gradual, meaning people with type 1 diabetes can still have surviving beta cells for some time after diagnosis. Dr Cantley hopes to find a way to make these remaining beta cells rapidly reproduce, a process called proliferation. Dr Cantley explained that a molecule called DYRK1A can trigger this process in the lab, and he plans to test this in mice with diabetes next. Dr Cantley said that to measure how well the treatment works, he’s building a huge microscope to view the whole mouse pancreas in high quality.
Dr Cantley said:
“This funding is a game-changer for innovative exploratory early research projects.”
Learn more about Dr Cantley’s Grand Challenge funded research.
Developing a protective coating for beta cells
Dr Vicky Salem was next to guide us through her vision for using biomaterials to keep beta cells safe from the immune attack in type 1 diabetes. Her team is developing a water-based jelly coating, known as a hydrogel, to protect lab-grown beta cells from the immune system once they’ve been transplanted into people with type 1. As well as acting as a protective shield, the aim is for the hydrogel to help connect beta cells to a blood supply so they can thrive after transplantation.
Dr Salem was joined by research team member PhD student Rea Tresa, who explained the sophisticated approach to encapsulating (coating) beta cells in the hydrogel, which involves 3D bioprinting. Oil and water are squirted together to form coatings around clusters of beta cells called islets, which then flow through a complex structure of cells and hydrogels which supports a blood supply but does not give access to the immune system.
Dr Salem said:
“Fellowships like this one support clinicians to engage with science for the benefit of patients.”
Learn more about Dr Salem’s Grand Challenge funded research.
Are islets surrendering or fighting back?
Professor Sarah Richardson was the last to share her research updates. Her project has three goals: to better understand how islets are attacked; to enhance islets’ defences; and to help other research groups to bridge the gap between the lab and the clinic, by validating their findings in human pancreases.
By examining rare human pancreas samples in incredible detail, Professor Richardson and her team are currently investigating the role of the protective barrier that forms around islets when the pancreas is developing in early life. And how easily the immune system is able to break it down, depending on the age a person develops type 1 diabetes. The aim is to understand why type 1 diabetes tends to be more aggressive in people diagnosed before the age of 12 years.
Telling us more about islets’ defence mechanisms, Prof Richardson also explained that there’s a protein on the surface of islets called HLA1 which makes them visible to the immune system. Another type of HLA1 helps to protect the islets. Prof Richardson’s team has found how islets release this protective HLA1 protein and is working on how to harness this process to protect islets in people with type 1.
Prof Richardson said:
“We have examined more pancreas samples from people with type 1 diabetes than anywhere else in the world.”
Learn more about Professor Richardson’s Grand Challenge funded research.
Welcoming new faces
Collaboration and community are at the heart of the Grand Challenge, so we celebrated the latest researchers to join the team. We now support over 100 researchers and collaborators working across at least 30 institutions in the UK and further afield. And even more will be joining the race to find new treatments and a cure for type 1 later this year when we announce the outcomes of our latest funding calls.

Amplifying voices
Diabetes UK’s Patient and Public Involvement Lead and JDRF UK’s Director of Research Partnerships spoke at the conference about how the Grand Challenge is taking a pioneering approach to involvement. From its outset, the Grand Challenge has been committed to involving people with lived experience of type 1 diabetes in all stages of the research life cycle. This means we can be confident that the research we fund is important, meaningful, and has the biggest potential to transform the lives of people with type 1 diabetes.
We’re grateful to our Type 1 Diabetes Research Panel members, who generously give their time to help researchers better understand the reality of living with type 1, to optimise the design, delivery, and dissemination of their research.

Empowering tomorrow’s leaders
We were delighted to be joined by a handful of Young Leaders from Diabetes UK’s Together Type 1 programme, also funded by the Steve Morgan Foundation. Together Type 1 is a community for children and young people aged 11-25 living with type 1 diabetes, enabling them to make new friends, learn new skills, and build confidence.
We brought Grand Challenge researchers and Young Leaders together in conversation, and discussed everything from career advice to diabetes research that holds the most promise to improve lives. We’ll be hearing directly from the Young Leaders about their time at DUKPC in the coming weeks.
Accelerating faster
Excitement is building around the Grand Challenge as the pace picks up and more researchers join the race towards a cure for type 1 diabetes. After three packed days hearing the latest research updates, celebrating a growing scientific community, and empowering more people with type 1 to get involved, it’s clear the Grand Challenge is building momentum to move us closer towards a future where the relentless burden of type 1 diabetes is a thing of the past.
You may also be interested in
Research into replacing insulin-producing cells is advancing rapidly, with ‘arm pancreas’ trial announced
March 21, 2024
Using a technique co-invented by Professor Matthias Hebrok, one of the Grand Challenge Scientific Advisory Panel Vice Chairs, researchers are exploring a promising treatment for type 1 diabetes in a new clinical trial, involving transplanting insulin-producing beta cells into the forearm, creating an ‘arm pancreas’.
Revolutionising research into beta cell replacement
Globally, research focused on replacing insulin-producing beta cells, which are destroyed in type 1 diabetes, is advancing rapidly. US biotech company Minutia is developing technology for a new clinical trial, supported by three non-dilutive funders, California’s Stem Cell Agency, JDRF International, and the National Institute of Health, and is working collaboratively with the University of California, San Francisco, and Duke University.
The two-part trial involves transplanting clusters of islets, that contain insulin-producing beta cells, into the forearms of eight participants, creating an ‘arm pancreas’. In the first phase, cells from donors have been successfully transplanted, while the second phase aims to use cells grown in the lab from stem cells, in much larger quantities.
Co-founder of Minutia Professor Hebrok, at the Technical University of Munich and Helmholtz Munich, said that while islet transplants from donors have already seen success, there’s a critical shortage of donors, meaning that only a tiny fraction of people with type 1 diabetes can currently benefit from a transplant.
Professor Hebrok said:
“I think the stem cell-derived cells are a revolution. Of course, we’re at the very early stages. But we could generate as many cells as we would like, to treat a tremendous number of patients.”
A growing community
The Type 1 Diabetes Grand Challenge is investing £30 million into the most cutting-edge projects in beta cell therapies. The diabetes research community is optimistic about the field’s potential to end the constant insulin dosing and blood sugar monitoring that people living with type 1 diabetes currently have to endure.
Professor Hebrok is Vice Chair of the Grand Challenge Scientific Advisory Panel advising on the research stream focused on beta cell replacement therapies. With funding from the Grand Challenge, there are now more than 70 researchers and collaborators working to grow, replace, and protect beta cells, so that people with type 1 diabetes can make their own insulin again. It’s encouraging to see the beta cell research community grow, with more researchers exploring creative new approaches that are moving us closer to a cure for type 1 diabetes.
Dr Lucy Chambers, Head of Research Communications at Diabetes UK, said:
“Cutting-edge cell therapies that enable people with type 1 diabetes to make their own insulin again are within reach.
“While there’s still much work to do to get these into clinical practice, programmes such as the UK’s Type 1 Diabetes Grand Challenge, are bringing us closer to the day when living with type 1 diabetes no longer requires relentless, round-the-clock self-management, and short- and long-term complications are a thing of the past.”
You may also be interested in
Type 1 Diabetes Grand Challenge round-up 2023
December 14, 2023
The Type 1 Diabetes Grand Challenge is providing a vital boost for UK diabetes research to find new treatments and cures for type 1 diabetes, faster. We are rallying the brightest minds around the UK and beyond to find ways to transform quality-of-life for the millions of people worldwide who live with type 1.
During 2023, the values at the heart of the Grand Challenge, speed, innovation, collaboration and ambition, have been clear. We made our first funding awards to nine diabetes research teams with big ideas, investing over £18 million to accelerate progress. While we’ve also been building vital capability within the diabetes research landscape, and nurturing creativity and collaboration in our three research priorities.
Here, we highlight what we’ve made happen in 2023.
Readying the starting blocks
To ensure we fuel research with the greatest possible potential to change the lives of people with type 1 diabetes, we enlisted the help of the world’s leading type 1 diabetes research experts. They sit on our Scientific Advisory Panels and work tirelessly to make sure our funding calls attract the best researchers with the most promising ideas.
This year, we’ve launched five new calls – asking scientists to develop ambitious and innovative research proposals and apply for our funding in each of the three Grand Challenge areas.
In February, we launched the first of our funding calls to accelerate research into the root causes of type 1 and ways to replace insulin-making beta cells, so that new treatments can make a difference to people with type 1 diabetes sooner. Next, we announced our plans to establish a flag-ship beta cell production and distribution centre, to ensure a supply of stem cell-derived beta cells for researchers in the UK.
With ambition, innovation and collaboration at the heart of the Type 1 Diabetes Grand Challenge, later in the year we called on scientists to push boundaries even further. Our Novel Insulins funding call is currently open and calling for bold ideas and innovations in insulin-based medicines from both academics and small-medium sized businesses, working across a range of disciplines from biotechnology to pharmacology. While our Beta Cell Therapy Innovations call is open for applications too. It’s seeking high-risk, high-reward ideas and new perspectives to support visionary ideas that could transform the field if successful.
Building momentum and collaboration
To prepare the research community for the Grand Challenge’s new and exciting way of funding research, we hosted first-of-a-kind networking events.
In May we held a virtual symposium on novel insulins research. The symposium provided a platform for researchers, policy makers and industry experts from around the world to share insights and expertise on the latest breakthroughs in novel insulin therapies.
Then in November, we held a networking workshop with scientists with diverse expertise, designed to spark cross disciplinary collaborations and fresh ideas, with the potential to overcome the roadblocks holding back progress in beta cell therapy research.
£18 million awarded so far
The response from the scientific community this year has been staggering, giving our expert advisory panels of scientists and people with lived experience of type 1 plenty of pioneering proposals to rigorously scrutinise and review.
In March, we announced the first projects awarded by the Type 1 Diabetes Grand Challenge. £5 million went to three exceptional researchers, who become our first Senior Research Fellows. Dr James Cantley at the University of Dundee, will test new drugs to help people grow back their own beta cells. Dr Victoria Salem at Imperial College London,will develop a device that can be implanted into people with type 1 diabetes to deliver new beta cells. Professor Sarah Richardson at the University of Exeter, will explore how and why a person’s immune system destroys their own beta cells.
Then in December, we announced Grand Challenge funding of over £13 million for a further six research projects. Two of these projects will investigate how to tackle the immune system attack at the root of type 1 diabetes using promising new treatments, called immunotherapies, which could prevent or slow the condition. The remaining four projects will tackle the challenge of replacing insulin-producing beta cells. Three research teams will aim to improve the quality, functionality and survival of the beta cells we can develop in the lab, while the final team aim to make islet transplants from donors more effective.
Looking ahead to 2024
With the outstanding new research teams our funding has forged, in hand with wider collaborative community our panels, events and patient and public engagement work have built, the pace is set. In 2024, we’ll be announcing the first funding awards in the Novel Insulins research theme, along with the outcome of our call for innovative beta cell therapy ideas. We’ll also be reporting on progress from the groundbreaking research projects already underway. And we look forward to an exciting programme of activity that will continue to stimulate bold, innovative research at scale and create the change needed to improve the lives of millions of people with type 1 diabetes.
Keep your eye on the News and Views section of our website for live updates on the Grand Challenge.