In May, we were out and about at type 1 diabetes community events. First, the virtual peer support platform DiabetesChat held a Grand Challenge special, then members of the Steve Morgan Foundation led a session at the annual Talking About Diabetes event.
DiabetesChat Grand Challenge special
DiabetesChat’s fifth research event was all about the Type 1 Diabetes Grand Challenge. Liam Eaglestone, CEO of the Steve Morgan Foundation (SMF), kicked off with a short presentation about SMF and their £50 million investment in type 1 diabetes research. He explained how the Grand Challenge is disrupting the research landscape and accelerating us towards treatments and cures for type 1.

Panel Discussion
DiabetesChat co-host Mary Murphy chaired a panel discussion between the three Senior Research Fellows, Professor Sarah Richardson, Dr James Cantley and Dr Victoria Salem. Mary asked the researchers questions about the Grand Challenge, including how the partnership is supporting research into future therapies and cures for type 1.
Dr Salem said: “The Grand Challenge has given us the freedom to think disruptively and bring in new ideas from other fields.”
Dr Cantley answered: “This type of research is mission driven, allowing us to take risks to move the field forward, improving lives and finding cures.”
Professor Richardson said: “We are supporting the next generation of researchers and establishing the research infrastructure here in the UK. With fresh brains in the mix, the future is bright!”
Research presentations
Each researcher spoke about their research and the audience were able to ask questions. Dr Cantley explained how he is developing new treatments for type 1, Professor Richardson took us through her research into type 1 immunology, and Dr Salem described how she is creating a protective device for lab-grown beta cells.
Watch the recording of the Grand Challenge DiabetesChat.
Response from the community
Over five hundred people tuned in to the event live, with almost 2,000 watching the recording. One audience member said: “Sarah’s slides with the artwork has made me understand my T1D after almost 60 years of diagnosis. Next life, I want to be a researcher!” Another said: “Amazing insight and I’ve gained a lot of knowledge tonight about my T1D and what the future might hold.”
Tom Dean, who hosts DiabetesChat said: “It was a fabulous, interesting and informative evening and the feedback we have received from the community has been very positive. It has given people hope and great anticipation for a healthier future for us all.”
SMF at Talking About Diabetes
The Type 1 Diabetes Grand Challenge had a big presence at this year’s Talking About Diabetes (TAD) event in Liverpool, with members of Diabetes UK, JDRF UK and SMF all in attendance, both on and off the stage.

Photo of Liam (left) and Jack (right), courtesy of Marc Lungley.
Liam and Jack Eaglestone
Liam and his son Jack were diagnosed with type 1 diabetes just one year apart. The pair gave a joint talk at this year’s TAD event where they praised the advances in technology and those championing access to it. Both Liam and Jack use hybrid closed loop systems to manage their type 1. They shared how the system has helped stabilise their blood glucose levels, reduce diabetes burnout and improve their sleep.
Jack said: “I used to have to take around one day a week off school because my blood glucose levels were so unstable. I would have repeated hypos which made me fall unconscious, high ketones and vomiting. Then, hybrid closed loop made that all disappear. It was like a miracle.”
Liam added: “Technology is great – but it is not a cure. The Grand Challenge is seeking that cure, by bringing together some of the best and brightest brains in the type 1 research community.”
A message from Steve and Sally Morgan
Steve and Sally Morgan couldn’t be at TAD in person, so they shared a video sharing their personal connection to type 1 through Sally’s son, Hugo, which led to the SMF’s transformational £50 million investment in type 1 diabetes research.
Watch the video from the Morgans below.
You may also be interested in
What it’s like being an expert by experience in the Type 1 Diabetes Grand Challenge
May 31, 2024
David Mitchell lives with type 1 diabetes and is a member of the expert funding panel guiding the projects we will fund through the Novel Insulins challenge. Here, he explains his volunteer role on the panel, the importance of involving people with lived experience in research, and what he learnt from the experience.
The Grand Challenge has committed £15 million of funding for researchers to design the next generation of insulins to make managing type 1 diabetes less challenging. To ensure we fund the most promising projects that offer the most potential benefit for people with type 1, we asked researchers to pitch their project ideas to a panel of experts. In this blog, David shares his experience of being a lived experience member of this panel.
Novel insulins pitches
It was a privilege being part of the international panel of experts for the Novel Insulins Innovation Incubator, reviewing grant applications of up to £500,000. It was fascinating to hear the exciting ideas that the researchers presented to us. All the research ideas had a lot of viability behind them already – my role was to provide a lived experience voice to help maximise the projects’ impact on people with type 1.
Insights on living with type 1
I gave the researchers perspective on the day-to-day things I experience with type 1. While some aspects are relatively well understood, I can relay little quirks to people who don’t live with the condition. For example, I asked the researchers pitching their projects to explain how their new ideas for insulin would consider the varying levels of daily activities not just between individuals but in the same person on different days.
Some of the applicants provided more detail than others on how they would factor exercise into their designs, which helped us evaluate the projects. Encouraging the researchers and other panel members to think about the daily reality of life with type 1 and how that affects science is why it is so important to involve people with lived experience in research right from the start.
Drawing inspiration from other industries
This volunteer role is very different from my career working at a financial technology (fintech) company. In that industry, we approach things from a different position to traditional corporate companies, so I’ve been able to suggest alternative ways of doing things. For example, we bring people together in big ‘hackathon’ events, which foster collaborative problem-solving over a short space of time. There’s no reason this concept couldn’t be taken into the research lab. This made me feel like, as well as relaying my experiences, I was also adding value to the development of the science.
Giving hope to people with type 1
As a member of the panel, I learnt a lot about type 1 diabetes research. I heard how insulin treatment could be enhanced to take away the need to constantly pump more insulin in and could be simplified to just one injection a day or even a week. Throughout the day, I learnt about different ideas for insulins that reduce the risk of hypos – a reality people with type 1 like me have to deal with.
When you live with the daily grind of constant insulin injections and glucose monitoring, the possibility that these insulins could be developed and allow you to forget about type 1 for the day is fabulous. Some trials of novel insulins are ongoing in animals. Learning that research is happening at this level gives me hope this could translate to something meaningful for humans.
The Grand Challenge approaches research differently
The amount of money the Grand Challenge is investing in type 1 diabetes research is fantastic. Being a panel member opened my eyes to how this injection of funding will lead to amazing research and accelerate developments. The substantial funding means scientists aren’t just working on a concept, it’s taking those ideas forward to unlock real progress and new treatments. It also attracts the interest of top experts from around the world to build on their amazing existing work.
I saw how the approach the Grand Challenge takes is different to typical research funding, which can be a long process. The Grand Challenge is structured to ensure that research ideas are turned into real action and meaningful change as soon as possible, while maintaining the scientific rigor.
Together Type 1 Young Leaders at DUKPC
May 28, 2024
In April, we were delighted to be joined at the Diabetes UK Professional Conference by seven Young Leaders from the Together Type 1 programme. With funding from the Steve Morgan Foundation, the UK-wide programme aims to bring together young people aged 11-25 years with type 1 diabetes, providing them with a platform to build confidence, learn new skills, and meet others in their region living with the condition.
The Young Leaders had a very busy schedule during the conference, attending key scientific sessions, interviewing Grand Challenge researchers, and sharing their own lived experience of type 1 diabetes with scientists and healthcare professionals alike. We’re grateful to two of them for taking the time to write about their first DUKPC experience.
Young Leader Elise Featherstone from the North team shared her reflections:
“A key presence at this year’s conference was the Type 1 Grand Challenge. Hearing about this research programme made me consider, for the first time, the reality of not having type 1 diabetes for the rest of my life. A cure may be sooner than we think, and it may well be because of the Grand Challenge!”
Bringing back beta cells
Dr James Cantley, a Grand Challenge Senior Research Fellow, optimistically shared findings from his team who are working to grow back insulin-making beta cells directly in the pancreas. Even during its early stages, this research offers hope and optimism for the diabetes community that one day we will be able to have functioning beta cells again.
New homes for transplanted cells
Dr Vicky Salem and Rea Tresa highlighted their lab’s work on bio-printing a protective housing unit to protect the life-saving transplanted beta cells. This project aims to make sure that new beta cells placed in the body are able to thrive and adapt. The Grand Challenge’s ability to bring great people and cutting-edge innovations together to accelerate life changing research is very exciting.
The type 1 timeline
Professor Sarah Richardson explained that as well as a cure for people with type 1 diabetes, we also need ways to prevent the condition from ever occurring in people at high risk. Prof Richardson shared her team’s work looking into rare pancreas samples. Obtaining these samples is difficult but has enabled Prof Richardson and her team to learn more around the type 1 diabetes timeline and how we may be able to prevent or intercept the immune system attack in type 1. Such a breakthrough could completely alter the implications of diabetes on society, our healthcare system, and end type 1 altogether for future generations.
Next Amelia Trencher from the Midlands and Eastern team summed up her thoughts:
“It was so wonderful to have the opportunity to attend DUKPC 2024 as a Young Leader, and to be able to have conversations with people who really wanted to hear about our experiences as young people living with type 1 diabetes.”
Scientific sessions
The collaboration between Together Type 1 and the Grand Challenge was a real highlight for all of us Young Leaders. I really enjoyed hearing the researcher I interviewed talk about his work and the impact he hoped it would have.
The main session about the Grand Challenge was really insightful and made us feel positive looking towards the future of life with type 1 diabetes. The main takeaways for me were that the big focus at the moment is on developing ways to give people with type 1 new beta cells, which seems to be very promising, moving towards a potential cure for type 1 in the reachable future.
Some researchers also talked about how they can use lessons learned from research into cancer and apply that to the diabetes research, which was very interesting to hear. It was also emphasised how important funding is for these projects.
Building networks
The Young Leaders were so pleased to meet Steve and Sally Morgan and to chat about how we have each benefited from being part of the Together Type 1 programme so far, and it was really lovely to see how much they cared about the personal impact of the programme of the lives of Young Leaders, not just the achievements and events that have taken place.
We also got to spend time with others who have lived experience of diabetes, and really enjoyed our joint session with the Dedoc voices, an international group diabetes advocates. It was also brilliant to just spend time with the other Young Leaders, as we had never met before, and by the end of the few days it felt like we’d been friends for ages.
The importance of the patient voice
On the second day, I was part of a panel discussion session about the first year of care for young people with diabetes. Not only was it such an honour to share the panel with some really inspiring people, but I also loved being able to have conversations during and after the session about the potential barriers for young people receiving optimal care.
I also had conversations with people about the mental burden of type 1 diabetes, including technology, which isn’t always considered by healthcare professionals, and can definitely be a barrier to optimal care.
Across the three days, I was so happy to see how engaged healthcare professionals were when talking to us about ways things could be improved in clinic, as well as realising how valuable our contributions can be in developing resources and programmes for other young people with type 1 diabetes.
In the future, I would love to see even more of a presence of young people at conferences, and in other spaces like DUKPC, and for more opportunities to meet and talk to researchers about their work, as this is something we don’t often get to do!
We’re grateful to Elise and Amelia for sharing what they did and learned while they were at DUKPC. It’s clear the Grand Challenge offers fresh hope to people living with type 1 diabetes.
You may also be interested in
The Type 1 Diabetes Grand Challenge returns to DUKPC
May 7, 2024
The Type 1 Diabetes Grand Challenge was the topic on everyone’s lips at this year’s Diabetes UK Professional Conference. Many of the large and growing community of Grand Challenge researchers were in attendance to celebrate their awards and update delegates on their research plans and progress.
The drive behind the Grand Challenge
The Grand Challenge session at this year’s DUKPC was chaired by Sally Morgan, a Trustee of the Steve Morgan Foundation, who opened with an emotive speech about her family’s journey with type 1 diabetes and their hope for a cure, and Professor Simon Heller, Chair of our Scientific Advisory Panels, who introduced the speakers, our three Senior Research Fellows.
Regrowing new beta cells
First up was Dr James Cantley, who began by explaining his ambitious drug discovery work to find a drug to regenerate the beta cells that have been destroyed by the immune attack. Sometimes the process of making new beta cells (neogenesis) is restored in adults, as a result of stress or injury. Dr Cantley and his team at the University of Dundee are modelling this process in the lab, and testing the effect different drugs have on it. Their aim is to find a drug that can support beta cell regrowth and be tested in clinical trials of people with type 1 diabetes.
Dr Cantley is also exploring how to encourage existing beta cells to reproduce. The immune attack on beta cells is gradual, meaning people with type 1 diabetes can still have surviving beta cells for some time after diagnosis. Dr Cantley hopes to find a way to make these remaining beta cells rapidly reproduce, a process called proliferation. Dr Cantley explained that a molecule called DYRK1A can trigger this process in the lab, and he plans to test this in mice with diabetes next. Dr Cantley said that to measure how well the treatment works, he’s building a huge microscope to view the whole mouse pancreas in high quality.
Dr Cantley said:
“This funding is a game-changer for innovative exploratory early research projects.”
Learn more about Dr Cantley’s Grand Challenge funded research.
Developing a protective coating for beta cells
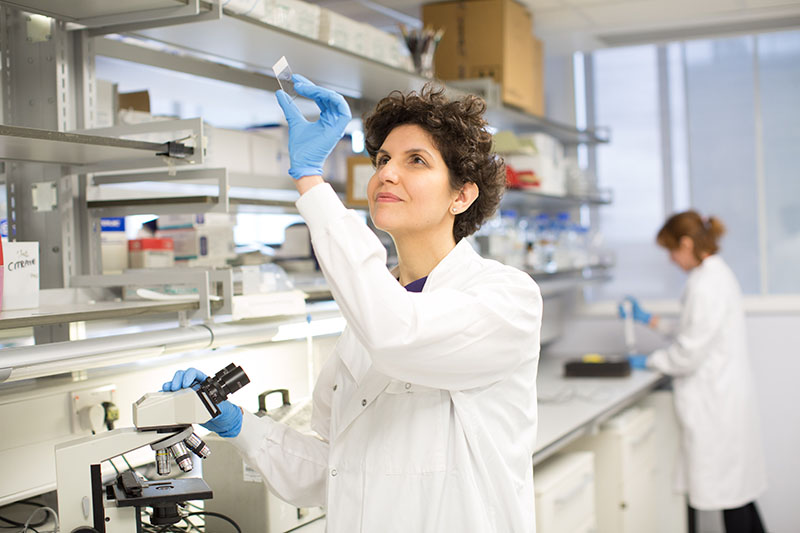
Dr Vicky Salem was next to guide us through her vision for using biomaterials to keep beta cells safe from the immune attack in type 1 diabetes. Her team is developing a water-based jelly coating, known as a hydrogel, to protect lab-grown beta cells from the immune system once they’ve been transplanted into people with type 1. As well as acting as a protective shield, the aim is for the hydrogel to help connect beta cells to a blood supply so they can thrive after transplantation.
Dr Salem was joined by research team member PhD student Rea Tresa, who explained the sophisticated approach to encapsulating (coating) beta cells in the hydrogel, which involves 3D bioprinting. Oil and water are squirted together to form coatings around clusters of beta cells called islets, which then flow through a complex structure of cells and hydrogels which supports a blood supply but does not give access to the immune system.
Dr Salem said:
“Fellowships like this one support clinicians to engage with science for the benefit of patients.”
Learn more about Dr Salem’s Grand Challenge funded research.
Are islets surrendering or fighting back?
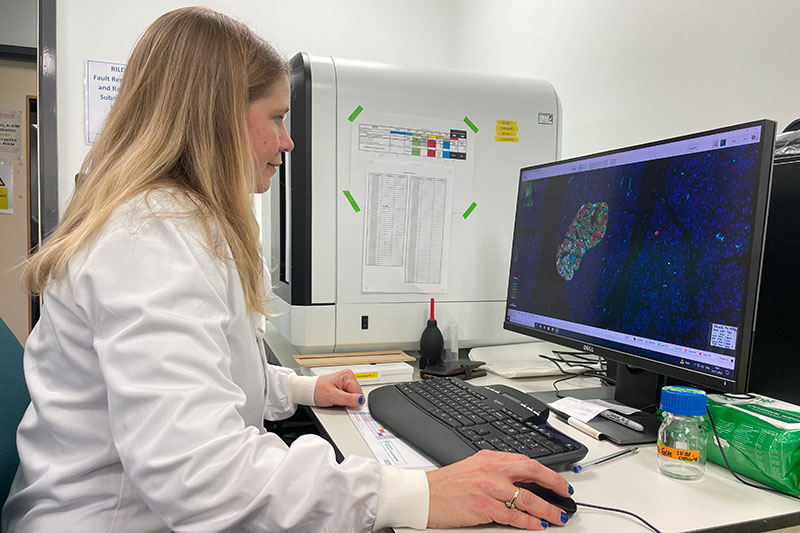
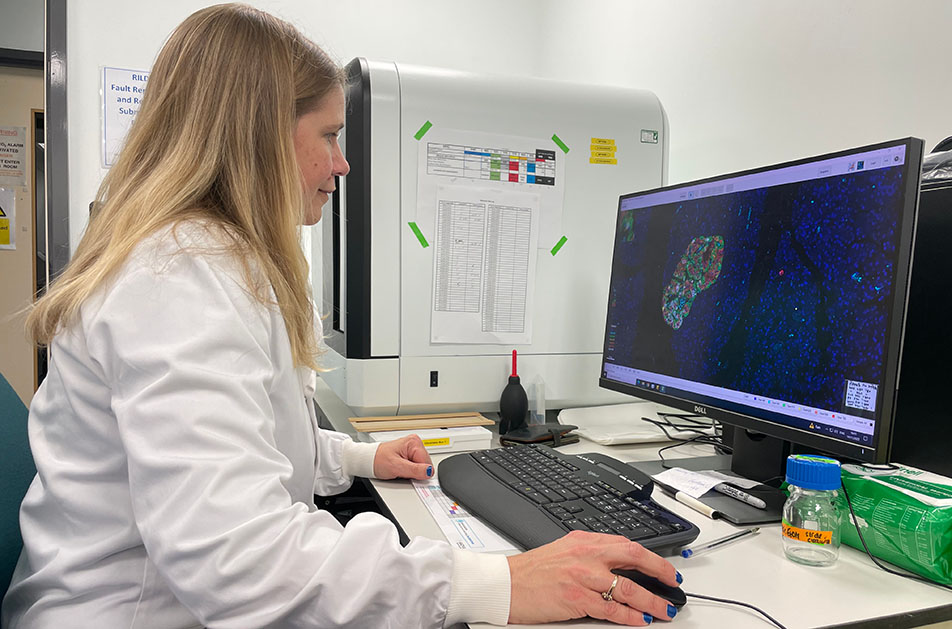
Professor Sarah Richardson was the last to share her research updates. Her project has three goals: to better understand how islets are attacked; to enhance islets’ defences; and to help other research groups to bridge the gap between the lab and the clinic, by validating their findings in human pancreases.
By examining rare human pancreas samples in incredible detail, Professor Richardson and her team are currently investigating the role of the protective barrier that forms around islets when the pancreas is developing in early life. And how easily the immune system is able to break it down, depending on the age a person develops type 1 diabetes. The aim is to understand why type 1 diabetes tends to be more aggressive in people diagnosed before the age of 12 years.
Telling us more about islets’ defence mechanisms, Prof Richardson also explained that there’s a protein on the surface of islets called HLA1 which makes them visible to the immune system. Another type of HLA1 helps to protect the islets. Prof Richardson’s team has found how islets release this protective HLA1 protein and is working on how to harness this process to protect islets in people with type 1.
Prof Richardson said:
“We have examined more pancreas samples from people with type 1 diabetes than anywhere else in the world.”
Learn more about Professor Richardson’s Grand Challenge funded research.
Welcoming new faces
Collaboration and community are at the heart of the Grand Challenge, so we celebrated the latest researchers to join the team. We now support over 100 researchers and collaborators working across at least 30 institutions in the UK and further afield. And even more will be joining the race to find new treatments and a cure for type 1 later this year when we announce the outcomes of our latest funding calls.

Amplifying voices
Diabetes UK’s Patient and Public Involvement Lead and JDRF UK’s Director of Research Partnerships spoke at the conference about how the Grand Challenge is taking a pioneering approach to involvement. From its outset, the Grand Challenge has been committed to involving people with lived experience of type 1 diabetes in all stages of the research life cycle. This means we can be confident that the research we fund is important, meaningful, and has the biggest potential to transform the lives of people with type 1 diabetes.
We’re grateful to our Type 1 Diabetes Research Panel members, who generously give their time to help researchers better understand the reality of living with type 1, to optimise the design, delivery, and dissemination of their research.

Empowering tomorrow’s leaders
We were delighted to be joined by a handful of Young Leaders from Diabetes UK’s Together Type 1 programme, also funded by the Steve Morgan Foundation. Together Type 1 is a community for children and young people aged 11-25 living with type 1 diabetes, enabling them to make new friends, learn new skills, and build confidence.
We brought Grand Challenge researchers and Young Leaders together in conversation, and discussed everything from career advice to diabetes research that holds the most promise to improve lives. We’ll be hearing directly from the Young Leaders about their time at DUKPC in the coming weeks.
Accelerating faster
Excitement is building around the Grand Challenge as the pace picks up and more researchers join the race towards a cure for type 1 diabetes. After three packed days hearing the latest research updates, celebrating a growing scientific community, and empowering more people with type 1 to get involved, it’s clear the Grand Challenge is building momentum to move us closer towards a future where the relentless burden of type 1 diabetes is a thing of the past.
You may also be interested in
Research into replacing insulin-producing cells is advancing rapidly, with ‘arm pancreas’ trial announced
March 21, 2024
Using a technique co-invented by Professor Matthias Hebrok, one of the Grand Challenge Scientific Advisory Panel Vice Chairs, researchers are exploring a promising treatment for type 1 diabetes in a new clinical trial, involving transplanting insulin-producing beta cells into the forearm, creating an ‘arm pancreas’.
Revolutionising research into beta cell replacement
Globally, research focused on replacing insulin-producing beta cells, which are destroyed in type 1 diabetes, is advancing rapidly. US biotech company Minutia is developing technology for a new clinical trial, supported by three non-dilutive funders, California’s Stem Cell Agency, JDRF International, and the National Institute of Health, and is working collaboratively with the University of California, San Francisco, and Duke University.
The two-part trial involves transplanting clusters of islets, that contain insulin-producing beta cells, into the forearms of eight participants, creating an ‘arm pancreas’. In the first phase, cells from donors have been successfully transplanted, while the second phase aims to use cells grown in the lab from stem cells, in much larger quantities.
Co-founder of Minutia Professor Hebrok, at the Technical University of Munich and Helmholtz Munich, said that while islet transplants from donors have already seen success, there’s a critical shortage of donors, meaning that only a tiny fraction of people with type 1 diabetes can currently benefit from a transplant.
Professor Hebrok said:
“I think the stem cell-derived cells are a revolution. Of course, we’re at the very early stages. But we could generate as many cells as we would like, to treat a tremendous number of patients.”
A growing community
The Type 1 Diabetes Grand Challenge is investing £30 million into the most cutting-edge projects in beta cell therapies. The diabetes research community is optimistic about the field’s potential to end the constant insulin dosing and blood sugar monitoring that people living with type 1 diabetes currently have to endure.
Professor Hebrok is Vice Chair of the Grand Challenge Scientific Advisory Panel advising on the research stream focused on beta cell replacement therapies. With funding from the Grand Challenge, there are now more than 70 researchers and collaborators working to grow, replace, and protect beta cells, so that people with type 1 diabetes can make their own insulin again. It’s encouraging to see the beta cell research community grow, with more researchers exploring creative new approaches that are moving us closer to a cure for type 1 diabetes.
Dr Lucy Chambers, Head of Research Communications at Diabetes UK, said:
“Cutting-edge cell therapies that enable people with type 1 diabetes to make their own insulin again are within reach.
“While there’s still much work to do to get these into clinical practice, programmes such as the UK’s Type 1 Diabetes Grand Challenge, are bringing us closer to the day when living with type 1 diabetes no longer requires relentless, round-the-clock self-management, and short- and long-term complications are a thing of the past.”
You may also be interested in
“It’s an optimistic time for people with type 1” – Morgan Shaw, a Grand Challenge researcher who has type 1
February 1, 2024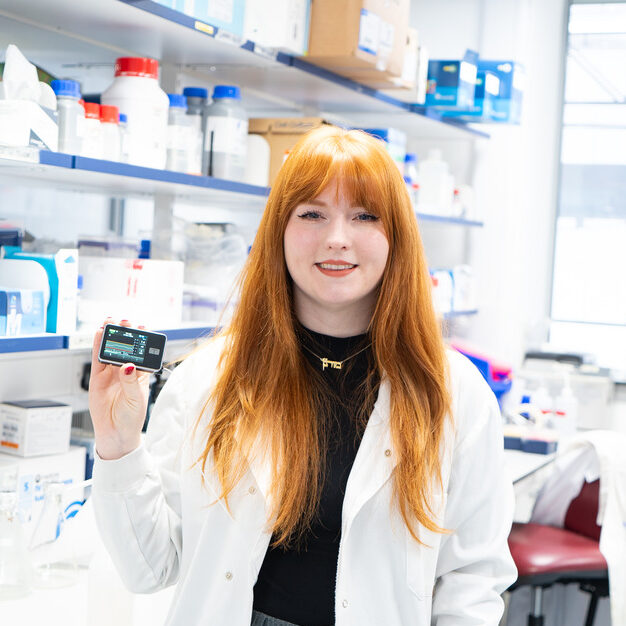
Research Technician Morgan Shaw has type 1 diabetes and is working in Dr James Cantley’s lab at the University of Dundee, which is funded by his Type 1 Diabetes Grand Challenge Senior Research Fellowship. Morgan tells us how collaboration, ambition and people with type 1 are at the heart of the Grand Challenge.
My type 1 diabetes
I was diagnosed with type 1 when I was 14, just before my first GCSE exam. My Dad researches type 1 diabetes and my mum lives with type 1, so they caught my symptoms of weight loss and extreme thirst before any permanent damage was caused. I’m currently using a closed loop system to manage my type 1 and I really like it. The system reduces the burden of type 1 and the variability in my blood glucose levels. This technology means I can get on with my day and work as anyone else would except for having a can of cola on my desk. The pump has also made my condition less visible to my colleagues as I don’t have to treat my hypos as often or give myself insulin injections.
Helping others with type 1
I’ve always been interested in science. At first, I wanted to be a vet, but having my own medical conditions pushed me to human science and helping other patients. I really enjoy being a lab technician because it’s a more hands-on approach to science. I like working with my hands and having a routine in the lab. Despite not being in direct contact with patients, I still have a sense that I’m helping other people living with type 1.
Giving our research perspective
Having diabetes and working on a type 1 specific project is really exciting. It gives me a different view and helps me focus on what people with type 1 need and want. It also helps me motivate the research team during long, hard lab days because knowing the end goal pushes us through. As a biomedical research lab, working with cells, tissues and models, we can feel separate from patients but having my perspective helps us. For example, I help scientists who aren’t used to speaking directly to people with type 1 to make sure the language they use in their presentations has the sensitivity and best phrasing for people with diabetes to read.
Teamwork in the Grand Challenge
I love working with the team in Dr James Cantley’s lab. We have lots of collaborators with different expertise working on different projects, so I get to see the other research taking place. We have lab meetings every week and scientific journal clubs to discuss newly published research papers. The Grand Challenge has a really collaborative feel, and we’re invited to attend a variety of different meetings. I’ve been given lots of responsibility as a technician and treated the same as the postdoctoral researchers, which isn’t always the case in other labs. James appreciates that we need a range of people with a variety of diverse opinions to achieve the most success.
Boosting Scottish diabetes research
It’s great to see a Northern lab in the UK being recognised by the Grand Challenge and receiving this funding. I wanted to work in Scotland and have been following James Cantley’s research closely. In my previous lab, I gained experience processing and studying human pancreatic organs generously donated for diabetes research. In James’ lab, we use a range of different cell and tissue approaches to progress our research, which means we can work faster and more flexibly towards new treatments.
Regrowing a person’s own beta cells
We’re studying pancreatic cell types which don’t make insulin to explore whether these can be converted into insulin-producing cells in people with type 1. The lab is exploring how the insulin-producing beta cells are related in embryos to another pancreatic cell type – the ductal cell. Dr Lisa Logie (a postdoctoral researcher) and I are optimising ductal cell isolation and culture, before other scientists in our team will add different drugs to see if they can transform them into beta cells.
A great research opportunity
I was following the Type 1 Diabetes Grand Challenge before I started working in James’ lab. It’s a very exciting time for type 1 diabetes research. The unprecedented amount of funding very generously invested by the Steve Morgan Foundation is making science a lot more open and available to more people. Being an early career researcher, working on this high-profile project is a great opportunity for me to learn new techniques and become more specialised. I’ll be working on this research project for its five-year duration. This gives me job security and the chance to focus and commit to this one project, which is very unusual in academic research.
A cure for type 1 diabetes
No one person with type 1 is the same as another, so we need to make sure there are treatment options for everyone. To me, a real cure for type 1 would be not having to administer insulin or wear a pump. I want to have a normal experience of life without having to think about type 1 with every aspect of my day.
Developing a cure for type 1 is the goal, but in the short-term, we need to keep making progress towards better quality of life for people with type 1. Making inulin pumps more sensitive and reducing the amount of insulin needed would be helpful, which is where the novel insulins strand of the Grand Challenge comes in.
Five-year research plan
Over the next five years it will be important to test different ideas, to evaluate which work and which don’t so that we can adapt our thinking and move forward towards our goal. Our aim is to develop a new treatment concept for type 1 by the end of the current Grand Challenge Fellowship, which we hope will then progress toward clinical trials.
You may also be interested in
Type 1 Diabetes Grand Challenge round-up 2023
December 14, 2023
The Type 1 Diabetes Grand Challenge is providing a vital boost for UK diabetes research to find new treatments and cures for type 1 diabetes, faster. We are rallying the brightest minds around the UK and beyond to find ways to transform quality-of-life for the millions of people worldwide who live with type 1.
During 2023, the values at the heart of the Grand Challenge, speed, innovation, collaboration and ambition, have been clear. We made our first funding awards to nine diabetes research teams with big ideas, investing over £18 million to accelerate progress. While we’ve also been building vital capability within the diabetes research landscape, and nurturing creativity and collaboration in our three research priorities.
Here, we highlight what we’ve made happen in 2023.
Readying the starting blocks
To ensure we fuel research with the greatest possible potential to change the lives of people with type 1 diabetes, we enlisted the help of the world’s leading type 1 diabetes research experts. They sit on our Scientific Advisory Panels and work tirelessly to make sure our funding calls attract the best researchers with the most promising ideas.
This year, we’ve launched five new calls – asking scientists to develop ambitious and innovative research proposals and apply for our funding in each of the three Grand Challenge areas.
In February, we launched the first of our funding calls to accelerate research into the root causes of type 1 and ways to replace insulin-making beta cells, so that new treatments can make a difference to people with type 1 diabetes sooner. Next, we announced our plans to establish a flag-ship beta cell production and distribution centre, to ensure a supply of stem cell-derived beta cells for researchers in the UK.
With ambition, innovation and collaboration at the heart of the Type 1 Diabetes Grand Challenge, later in the year we called on scientists to push boundaries even further. Our Novel Insulins funding call is currently open and calling for bold ideas and innovations in insulin-based medicines from both academics and small-medium sized businesses, working across a range of disciplines from biotechnology to pharmacology. While our Beta Cell Therapy Innovations call is open for applications too. It’s seeking high-risk, high-reward ideas and new perspectives to support visionary ideas that could transform the field if successful.
Building momentum and collaboration
To prepare the research community for the Grand Challenge’s new and exciting way of funding research, we hosted first-of-a-kind networking events.
In May we held a virtual symposium on novel insulins research. The symposium provided a platform for researchers, policy makers and industry experts from around the world to share insights and expertise on the latest breakthroughs in novel insulin therapies.
Then in November, we held a networking workshop with scientists with diverse expertise, designed to spark cross disciplinary collaborations and fresh ideas, with the potential to overcome the roadblocks holding back progress in beta cell therapy research.
£18 million awarded so far
The response from the scientific community this year has been staggering, giving our expert advisory panels of scientists and people with lived experience of type 1 plenty of pioneering proposals to rigorously scrutinise and review.
In March, we announced the first projects awarded by the Type 1 Diabetes Grand Challenge. £5 million went to three exceptional researchers, who become our first Senior Research Fellows. Dr James Cantley at the University of Dundee, will test new drugs to help people grow back their own beta cells. Dr Victoria Salem at Imperial College London,will develop a device that can be implanted into people with type 1 diabetes to deliver new beta cells. Professor Sarah Richardson at the University of Exeter, will explore how and why a person’s immune system destroys their own beta cells.
Then in December, we announced Grand Challenge funding of over £13 million for a further six research projects. Two of these projects will investigate how to tackle the immune system attack at the root of type 1 diabetes using promising new treatments, called immunotherapies, which could prevent or slow the condition. The remaining four projects will tackle the challenge of replacing insulin-producing beta cells. Three research teams will aim to improve the quality, functionality and survival of the beta cells we can develop in the lab, while the final team aim to make islet transplants from donors more effective.
Looking ahead to 2024
With the outstanding new research teams our funding has forged, in hand with wider collaborative community our panels, events and patient and public engagement work have built, the pace is set. In 2024, we’ll be announcing the first funding awards in the Novel Insulins research theme, along with the outcome of our call for innovative beta cell therapy ideas. We’ll also be reporting on progress from the groundbreaking research projects already underway. And we look forward to an exciting programme of activity that will continue to stimulate bold, innovative research at scale and create the change needed to improve the lives of millions of people with type 1 diabetes.
Keep your eye on the News and Views section of our website for live updates on the Grand Challenge.
You may also be interested in
Type 1 Diabetes Grand Challenge invests £13 million into six transformational new projects
December 7, 2023
We’re thrilled to unveil the latest groundbreaking research projects funded by the Type 1 Diabetes Grand Challenge. Earlier this year, we called on scientists to submit research proposals to get us closer to having new treatments for people with type 1 diabetes that tackle the root cause of their condition and restore their insulin-making beta cells.
Now, over £13 million of funding will support six outstanding research teams – made up of 49 scientists, working at 22 different institutions in the UK and Europe – to fast-track discoveries that could see us make huge strides in how we treat type 1 diabetes.
Helping people make their own insulin
To cure type 1 diabetes, we need to find a way to give people with type 1 diabetes new beta cells that work to precisely control their blood sugar levels. Four of our new projects will innovate new ways of reaching this goal.
Beta cells: replace, protect, regenerate
Professor David Hodson, at University of Oxford, Dr Ildem Akerman, at University of Birmingham, and Dr Johannes Broichhagen, at Leibniz FMP, will lead a team to explore how insulin-boosting molecules that sit on the surface of beta cells could be harnessed to create beta cells in the lab that work better and survive for longer.
They’ll also investigate if the molecules can be used to deliver treatments that help to protect transplanted beta cells from the immune system or trigger new beta cells to grow inside the body, by encouraging other cells in the pancreas to transform into beta cells.
Find out more about the team’s project.
Bolstering beta cells ready for transplantation
Professor Shanta Persaud and Dr Aileen King, at King’s College London, and team will work to create an unlimited supply of elite beta cells ready for transplant. They’ll draw on their expert knowledge in how the human pancreas works and develops, and apply this to making beta cells from stem cells in the lab. As they grow their beta cells, they’ll bolster them with specialised support cells and helpful nutrients that will encourage them to fully develop so they can respond to changing blood sugar levels just as well as real beta cells do.
Find out more about the team’s project.
Creating a better home for transplanted beta cells
Professor Francesca Spagnoli and Dr Rocio Sancho at King’s College London, together with Professor Molly Stevens at University of Oxford, will focus on ways to keep lab-made beta cells safe from harm. They’ll use cutting-edge technology to boost beta cells’ chances of survival once transplanted by coating them with protective gels and using nanoparticle technology to create a synthetic microenvironment to protect them from stress and immune attack.
The team will also develop a transplantation device that beta cells can live inside, to protect them from the hostile environment they’ll face once transplanted inside the body.
Find out more about the team’s project.
Unleashing the benefits of cell transplants
Professor Shareen Forbes, at University of Edinburgh, and Dr Lisa White, at University of Nottingham, will spearhead a team to search for ways to boost the benefits of donor beta cells transplants (called islet transplants). They’ll investigate if delivering drugs packaged inside microcapsules alongside islet transplants helps the donated beta cells produce more insulin and survive for longer. This would make islets transplants more effective and mean many more people with type 1 diabetes could benefit.
Finally, the team will investigate if this approach could be applied to beta cells made from stem cells.
Find out more about the team’s project.
Stopping the immune attack’s harm
In people living with type 1 diabetes, the immune system remains primed to seek out and destroy beta cells. To ensure the survival of any new beta cells transplanted into people with type 1, protection from the immune system is critical. Two projects from our latest multi-million-pound investment are focused on promising new immunotherapy treatments, which fend off the immune attack in type 1 diabetes.
Immunotherapy: is timing everything?
Dr James Pearson, at Cardiff University, and his team will investigate if the time of day when we give an immunotherapy can affect how well it works. They’ll study a type of immunotherapy drug named interleukin-2 (IL-2). It works by expanding the population of helpful immune cells, called regulatory T cells (Tregs), which try to prevent killer immune cells from launching their attack. Dr Pearson has found evidence that Tregs respond differently to IL-2 depending on the time of day and will now explore this further.
The findings could help to improve the effectiveness of a promising immunotherapy for people with and at risk of type 1 diabetes by identifying the best time of day to give the treatment.
Find out more about the team’s project.
Are two immunotherapies better than one?
Dr Danijela Tatovic, at Cardiff University, will head a team to explore if combining two immunotherapies that target different parts of the immune system could make them more effective at protecting beta cells.
They’ll run a clinical trial testing the immunotherapies abatacept and IL-2 with people recently diagnosed with type 1 diabetes, who still have some surviving beta cells. Their findings will tell us how best to combine the drugs and will lay the groundwork for a bigger trial, which could build the evidence needed to make this combination treatment available for people with or at risk of type 1 diabetes.
Find out more about the team’s project.
Dr Elizabeth Robertson, Director of Research at Diabetes UK, said:
“We’re in a hugely exciting period for the Type 1 Diabetes Grand Challenge, as today we welcome six exceptional scientists who will lead exciting multi-disciplinary teams to drive forward this pioneering initiative and build momentum towards our ambitious goal.
“This announcement brings with it fresh hope of a cure for everyone living with type 1 diabetes, and we look forward to seeing how these projects will break new ground in our search for life-changing beta cell therapies and treatments to overcome the type 1 immune system attack.”
Rachel Connor, Director of Research Partnerships at JDRF UK, said:
“Today’s announcement of six newly funded research projects demonstrates the speed and ambition of the Type 1 Diabetes Grand Challenge. All six projects hold great promise for people with type 1 diabetes. We can’t wait to see the results of this vital research to transform beta cell therapy and tackle the immune reaction that is at the root of driving type 1.”
Steve and Sally Morgan, Founders of the Steve Morgan Foundation, said:
“This is an exciting moment in our partnership with Diabetes UK and JDRF UK. We are astounded by the innovation and vision of the new projects and look forward to seeing how the research helps us realise our ambition of transforming the lives of people with type 1 diabetes.”
Our latest awards take the total amount of funding the Type 1 Diabetes Grand Challenge has awarded in 2023 to over £18 million, following the Steve Morgan Foundation’s momentous £50 million pledge. We’ll keep you updated on the progress of this extraordinary research as our growing squad of scientists help us step closer to a cure.
You may also be interested in
£1 million available to ignite beta cell therapy innovations
December 5, 2023
Today sees the opening of a new Type 1 Diabetes Grand Challenge funding call focused on supporting innovations into beta cell therapies for people with type 1 diabetes.
Following our networking workshop last week, designed to spark cross disciplinary collaborations and fresh thinking into beta cell therapy research, we’re offering individual awards of up to £400,000. We want to support visionary research that will transform the field, by embracing high-risk, high-reward proposals. New and creative ideas that will address an unmet need in beta cell therapy research are strongly encouraged.
We also know that drawing on expertise from beyond type 1 diabetes could unlock innovations to overcome current obstacles. That’s why we’re encouraging multi-disciplinary collaboration and are calling on researchers from any discipline, including immunology, stem cell science, medicinal chemistry or bioengineering, to get involved.
Diabetes UK and JDRF have worked with the Grand Challenge Scientific Advisory Panels, comprising some of the world’s most eminent type 1 diabetes scientists, to shape this new call.
Apply for funding
Find out more and apply for the Beta Cell Therapy Innovation Project Grant.
Researchers will be asked to submit a brief research plan, including a short video pitch, by February 19th 2024. The very best applicants will then be invited to a virtual interview.
Diabetes UK and JDRF are passionate about working closely with people affected by type 1 diabetes and encourage all applicants to do the same when building their applications.
If you’re a researcher and want to learn more about the Beta Cell Therapy Innovation Project Grant call, including top tips for applying, sign up to our webinar on December 14th.
Professor Qizhi Tang, a member of our Scientific Advisory Panel on beta cell therapies, said:
“Recent advances in stem cell technology and cell engineering have provided an unprecedented opportunity to restore beta cell function in people with type 1 diabetes. The Type 1 Diabetes Grand Challenge is a momentous call to action to work together to advance this therapy.”
You may also be interested in
£1 million available to ignite beta cell therapy innovations
November 28, 2023
Today sees the opening of a new Type 1 Diabetes Grand Challenge funding call focused on supporting innovations into beta cell therapies for people with type 1 diabetes.
Following our networking workshop last week, designed to spark cross disciplinary collaborations and fresh thinking into beta cell therapy research, we’re offering individual awards of up to £400,000. We want to support visionary research that will transform the field, by embracing high-risk, high-reward proposals. New and creative ideas that will address an unmet need in beta cell therapy research are strongly encouraged.
We also know that drawing on expertise from beyond type 1 diabetes could unlock innovations to overcome current obstacles. That’s why we’re encouraging multi-disciplinary collaboration and are calling on researchers from any discipline, including immunology, stem cell science, medicinal chemistry or bioengineering, to get involved.
Diabetes UK and JDRF have worked with the Grand Challenge Scientific Advisory Panels, comprising some of the world’s most eminent type 1 diabetes scientists, to shape this new call.
Apply for funding
Find out more and apply for the Beta Cell Therapy Innovation Project Grant.
Researchers will be asked to submit a brief research plan, including a short video pitch, by February 19th 2024. The very best applicants will then be invited to a virtual interview.
Diabetes UK and JDRF are passionate about working closely with people affected by type 1 diabetes and encourage all applicants to do the same when building their applications.
If you’re a researcher and want to learn more about the Beta Cell Therapy Innovation Project Grant call, including top tips for applying, sign up to our webinar on December 14th.
Professor Qizhi Tang, a member of our Scientific Advisory Panel on beta cell therapies, said:
“Recent advances in stem cell technology and cell engineering have provided an unprecedented opportunity to restore beta cell function in people with type 1 diabetes. The Type 1 Diabetes Grand Challenge is a momentous call to action to work together to advance this therapy.”